Subtalar Joint
By : Najah SabahDefinition
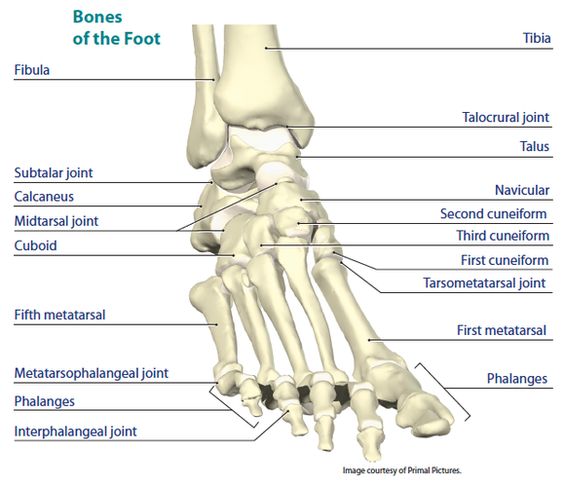
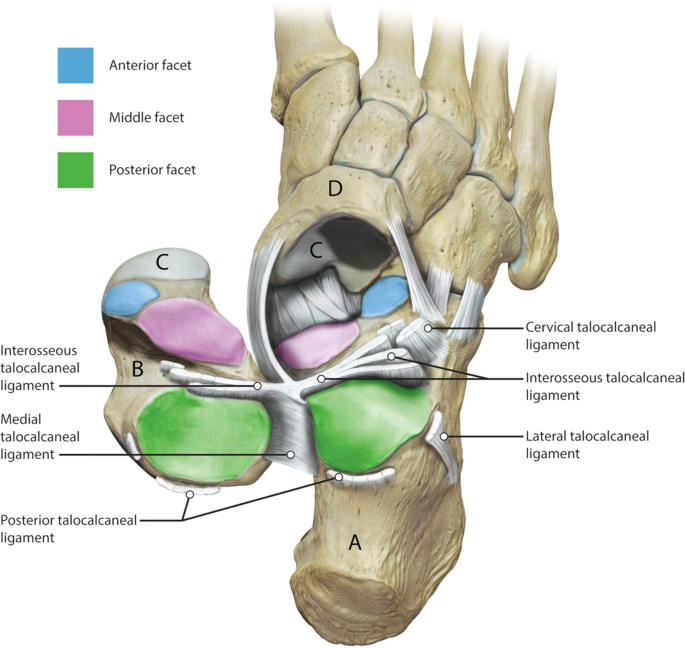
The subtalar joint is the posterior joint between the talus and the calcaneum. Articulation is between the inferior surface of the body of the talus and the facet on the middle of the upper surface of the calcaneum . The articular surfaces are covered with hyaline cartilage.(see figure 1)
Type
This is a plane joint.
Capsule
The capsule encloses the joint and is attached to the margins of the articular areas of the two bones.
Ligaments
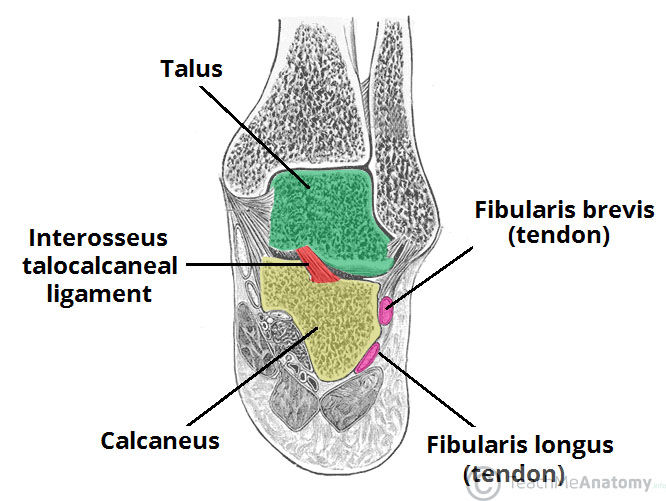
Medial and lateral (talocalcaneal) ligaments strengthen the capsule. Theinterosseous (talocalcaneal) ligament is strong and is the main bond of union between the two bones. It attaches above to the sulcus tali and below to the sulcus calcanei.(see figure 2)
Structure
The ST joint is multi-articular joint, with three articulated facets that provide a surface for the joint to glide:
1.The anterior subtalar joint : Allows joint to glide forward (anterior articulation)
2.The medial subtalar joint: Allows joint to glide side-to-side (eversion/inversion)
3.The posterior subtalar joint: Allows the to glide backward (posterior articulation).(see video 1)(see figure 2)
Synovial Membrane
The synovial membrane lines the capsule.
Function
The ST joint is key to many functional activities eg walking and running, and posture while performing these tasks. The mechanisms behind how the subtalar joint propels you us is very complex.
This ST joints primary movements involve supination, in which the foot rolls toward the body's midline, and pronation, in which the foot rolls away from the midline. Both of these movements require a combination of distinct actions.
•Pronation requires a combination of dorsiflexion, abduction, and eversion.
•Supination requires a combination of plantar flexion, adduction and inversion.
(see figure 3)
Movements
The movements that occur at the subtalar joint are gliding and rotation.The combination of these movements result in pronation and supination; these are considered to be the primary movements in the subtalar joint. They are always accompanied by movements in the talocalcaneonavicular and calcaneocuboid joints and as such these three joints are considered to be one functional unit of the foot.
1.Supination in the subtalar joint is primarily produced by tibialis anterior and tibialis posterior , with assistance from extensor hallucis longus, flexor hallucis longus and flexor digitorum longus .
2.Pronation is mainly produced by fibularis longus, fibularis brevis and fibularis tertius with assistance from the extrinsic muscles that extend the toes ( extensor digitorum longus and extensor hallucis longus ).
Neurovascular Supply
The subtalar joint receives supply from two arteries and two nerves. Arterial supply comes from the posterior tibial and fibular arteries .
Innervation to the plantar aspect of the joint is supplied by the medial or lateral plantar nerve , whereas the dorsal aspect of the joint is supplied by the deep fibular nerve .
Type
This is a plane joint.
Capsule
The capsule encloses the joint and is attached to the margins of the articular areas of the two bones.
Ligaments
Medial and lateral (talocalcaneal) ligaments strengthen the capsule. Theinterosseous (talocalcaneal) ligament is strong and is the main bond of union between the two bones. It attaches above to the sulcus tali and below to the sulcus calcanei.(see figure 2)
Structure
The ST joint is multi-articular joint, with three articulated facets that provide a surface for the joint to glide:
1.The anterior subtalar joint : Allows joint to glide forward (anterior articulation)
2.The medial subtalar joint: Allows joint to glide side-to-side (eversion/inversion)
3.The posterior subtalar joint: Allows the to glide backward (posterior articulation).(see video 1)(see figure 2)
Synovial Membrane
The synovial membrane lines the capsule.
Function
The ST joint is key to many functional activities eg walking and running, and posture while performing these tasks. The mechanisms behind how the subtalar joint propels you us is very complex.
This ST joints primary movements involve supination, in which the foot rolls toward the body's midline, and pronation, in which the foot rolls away from the midline. Both of these movements require a combination of distinct actions.
•Pronation requires a combination of dorsiflexion, abduction, and eversion.
•Supination requires a combination of plantar flexion, adduction and inversion.
(see figure 3)
Movements
The movements that occur at the subtalar joint are gliding and rotation.The combination of these movements result in pronation and supination; these are considered to be the primary movements in the subtalar joint. They are always accompanied by movements in the talocalcaneonavicular and calcaneocuboid joints and as such these three joints are considered to be one functional unit of the foot.
1.Supination in the subtalar joint is primarily produced by tibialis anterior and tibialis posterior , with assistance from extensor hallucis longus, flexor hallucis longus and flexor digitorum longus .
2.Pronation is mainly produced by fibularis longus, fibularis brevis and fibularis tertius with assistance from the extrinsic muscles that extend the toes ( extensor digitorum longus and extensor hallucis longus ).
Neurovascular Supply
The subtalar joint receives supply from two arteries and two nerves. Arterial supply comes from the posterior tibial and fibular arteries .
Innervation to the plantar aspect of the joint is supplied by the medial or lateral plantar nerve , whereas the dorsal aspect of the joint is supplied by the deep fibular nerve .
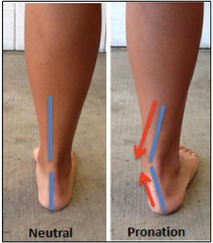
Ankle_Pronation_Position
Clinical Note
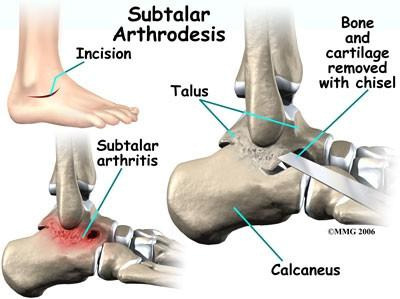
calcaneal fracture
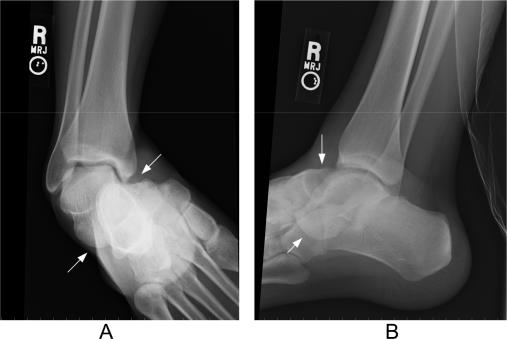
The calcaneus is often fractured in a ‘crush‘ type injury. The most common mechanism of damage is falling onto the heel from a height – the talus is driven into the calcaneus. The bone can break into several pieces, known as a comminuted fracture. Upon x-ray imaging, the calcaneus will appear shorter and wider.
A calcaneal fracture can cause chronic problems, even after treatment. The subtalar joint is usually disrupted, causing the joint to become arthritic. The patient will experience pain upon inversion and eversion – which can make walking on uneven ground particularly painful.(see figure 4)
The calcaneus is often fractured in a ‘crush‘ type injury. The most common mechanism of damage is falling onto the heel from a height – the talus is driven into the calcaneus. The bone can break into several pieces, known as a comminuted fracture. Upon x-ray imaging, the calcaneus will appear shorter and wider.
A calcaneal fracture can cause chronic problems, even after treatment. The subtalar joint is usually disrupted, causing the joint to become arthritic. The patient will experience pain upon inversion and eversion – which can make walking on uneven ground particularly painful.(see figure 4)

X-ray of a calcaneal fracture
Injuries
1-SUBTALAR JOINT PAIN AND “SINUS TARSI SYNDROME’’
What and where is it?
The joint below the ankle that connects the talus to the calcaneus. There are ligaments, nerves, fat and synovial lining that are susceptible to stress and injury.
What does the joint do?
The subtalar joint allows your foot to turn side-to-side and adapt to uneven surfaces. It is an important shock absorbing joint that helps prevent injuries and fractures to the leg and spine.
How do injuries occur?
• Twisting injuries that occur on uneven surfaces or during sports and activities.
• Motor vehicle accidents where the heel stays solid on the floorboard and the foot shifts over it.
• Running on uneven surfaces such as the beach or gravel when you are not accustomed to that.
• Slide tackles in soccer in which the foot is pointed down to an extreme.
• Falls from a height directly on your heel may cause fractures into the joint.
Signs and symptoms:
• Swelling may be present on the back or outside of the foot and the lower portion of the ankle.
• Possible loss of side-to-side motion.
• Pain and stiffness getting out of bed in the morning to walk. This may improve with weight bearing and then cause pain or a deep ache later on in the day.
• Inability to turn the foot side-to-side with comfort during a golf swing or tennis motion.
• Feeling of instability on uneven surfaces.
How are injuries diagnosed?
• A thorough history and physical examination of the lower extremity and foot.
• X-rays are taken to rule out fractures, tumors, osteoarthritis or joint misalignment.
• The possible ordering of MRIs to evaluate the ligaments, tendons, joint, bone marrow and surrounding soft tissue structures.
• Possible CT scans for a better evaluation of the bony structures.
Treatment:
• Conservative care for most injuries may include oral anti-inflammatories or Cortisone injections to reduce inflammation.
• Physical therapy to help strengthen surrounding muscles, improve joint range of motion and general lower extremity flexibility and balance.
• Orthotics made to go in your shoes to support the injured area, especially if the foot is very high or low arches.
• Arthroscopic surgery may be needed to clean out damaged tissue if conservative treatment fails. A 1/6” camera is placed in the side or back of the foot and small instruments are used to clean up the joint damage. If there is no arthritis, an excellent outcome is expected. If more damage is seen to the cartilage surface, bone cuts or joint fusions may be necessary. Still, the prognosis would be excellent.
*Prognosis is always going to be greatly improved if the condition is evaluated quickly and treated early.
(see video 2)(see figure 5)
The joint below the ankle that connects the talus to the calcaneus. There are ligaments, nerves, fat and synovial lining that are susceptible to stress and injury.
What does the joint do?
The subtalar joint allows your foot to turn side-to-side and adapt to uneven surfaces. It is an important shock absorbing joint that helps prevent injuries and fractures to the leg and spine.
How do injuries occur?
• Twisting injuries that occur on uneven surfaces or during sports and activities.
• Motor vehicle accidents where the heel stays solid on the floorboard and the foot shifts over it.
• Running on uneven surfaces such as the beach or gravel when you are not accustomed to that.
• Slide tackles in soccer in which the foot is pointed down to an extreme.
• Falls from a height directly on your heel may cause fractures into the joint.
Signs and symptoms:
• Swelling may be present on the back or outside of the foot and the lower portion of the ankle.
• Possible loss of side-to-side motion.
• Pain and stiffness getting out of bed in the morning to walk. This may improve with weight bearing and then cause pain or a deep ache later on in the day.
• Inability to turn the foot side-to-side with comfort during a golf swing or tennis motion.
• Feeling of instability on uneven surfaces.
How are injuries diagnosed?
• A thorough history and physical examination of the lower extremity and foot.
• X-rays are taken to rule out fractures, tumors, osteoarthritis or joint misalignment.
• The possible ordering of MRIs to evaluate the ligaments, tendons, joint, bone marrow and surrounding soft tissue structures.
• Possible CT scans for a better evaluation of the bony structures.
Treatment:
• Conservative care for most injuries may include oral anti-inflammatories or Cortisone injections to reduce inflammation.
• Physical therapy to help strengthen surrounding muscles, improve joint range of motion and general lower extremity flexibility and balance.
• Orthotics made to go in your shoes to support the injured area, especially if the foot is very high or low arches.
• Arthroscopic surgery may be needed to clean out damaged tissue if conservative treatment fails. A 1/6” camera is placed in the side or back of the foot and small instruments are used to clean up the joint damage. If there is no arthritis, an excellent outcome is expected. If more damage is seen to the cartilage surface, bone cuts or joint fusions may be necessary. Still, the prognosis would be excellent.
*Prognosis is always going to be greatly improved if the condition is evaluated quickly and treated early.
(see video 2)(see figure 5)
2-SUBTALAR DISLOCATION
Definition : A rare ankle injury that occurs with disruption of the talo-navicular and talocalcaneal joints. Not to be confused with “ankle” (tibio-talar) dislocation.(see figure 6)
Role of Subtalar Joint
• Provides shock absorption
• Permits foot to adjust to uneven ground (such as walking on sand)
Mechanism:
• High energy trauma
o Fall from height
o Motor vehicle accident
• Plantar flexed-foot (foot lands on ground while inverted or everted).
Classification/Physical Exam
• Open (up to 25%) vs. Closed
• Medial: ~60-80% (Weatherford, Yoder 2011)
o Inversion injury
o Foot locked in plantar flexion and supinated (Menkes 2000)
o Sometimes referred to as “basketball foot”as it is seen when basketball players land after jumping) (Yoder 2011)
o Head of talus prominent dorsolaterally
• Lateral
o Eversion injury
o Foot locked in pronation
o Because of surrounding anatomical structures, lateral dislocation requires more force; thus, more frequently open and/or associated with other injuries (Yoder 2011)
o Calcaneus is displaced lateral to talus
• Anterior (from hyperextension) /Posterior (from hyperflexion)
o Much less common (< 5% of all dislocations) (DeLee 1982)
Diagnostic Imaging
• Dislocations will be clear on plain radiographs
• X-ray
o Obtain AP and lateral views of foot and ankle
o Medial Dislocation: talar head superior to navicular on lateral image
o Lateral Dislocation: talar head colinear or inferior to navicular bone on lateral image, non-distinguishable subtalar joint.(see figure 7)
ED Management
• Complete a primary and secondary trauma survey looking for additional injuries
• Assess neurovascular status and perform skin exam
• Provide analgesia
• Consider early consultation with orthopedics
o These dislocations are often much more difficult to reduce than standard ankle dislocations (tibio-talar dislocations)
o Up to 32% of subtalar dislocations require open reduction (Bibbo 2003)
Medial reduction can be blocked by capsule of talonavicular joint and extensor digitorum brevis, deep peroneal neurovascular bundle, talar head can “buttonhole” through the extensor digitorum brevis, or impaction can occur on navicular
Lateral reduction can be blocked by posterior tibial tendon (most common), impaction fractures, or other tendons
• Reduction Approach
o Standard ankle reduction techniques can lead to further injury and morbidity
o Flex the patient’s knee (90 degrees) and hip to reduce tension on the gastrocnemius and hold counter-traction (you may require an assistant for this)
o Place the ankle in plantar flexion
o For MEDIAL dislocations, grasp calcaneus with dominant hand, dorsum of foot with opposite hand, for LATERAL dislocations, do the same but also place non-dominant thumb over navicular
o Distract the hindfoot and apply direct pressure to talar head while inverting vs. everting to exaggerate the deformity
If patient is inverted (medial dislocation), hyper-invert
If patient is inverted everted (lateral dislocation), hyper-evert
Subsequently reverse the direction of dislocation (Thompson 2011)
• Post-Reduction
o Post-reduction X-rays
Confirm proper alignment
Evaluate for osteochondral lesions (injuries and/or small fractures of cartilage surface of talus), compression fractures, and other injuries of ankle/foot
o Consider post-reduction CT scan (Yoder 2011, Bibbo 2003)
Concomitant foot/ankle injuries are common (88-100%)
These injuries may be missed on plain radiographs
CT findings may change management and may affect outcomes
Optimal time to obtain CT scan (ED vs as outpatient) is unknown
o Short leg cast, non-weight bearing for 3-6 weeks (may consider short leg posterior/AO splint in ED after reduction for presumed swelling with close ortho follow up to transition to cast) (DeLee JC 1982)
Complications
o Post-Traumatic Arthritis
o Small number of subtalar fusions
o Lateral dislocations typically fare worse (as above, higher-energy mechanism, more frequent concomitant injuries)
o Infection with open wounds
* watch this video Subtalar Dislocation - Everything You Need To Know - Dr. Nabil Ebraheim
(see video 3)
Role of Subtalar Joint
• Provides shock absorption
• Permits foot to adjust to uneven ground (such as walking on sand)
Mechanism:
• High energy trauma
o Fall from height
o Motor vehicle accident
• Plantar flexed-foot (foot lands on ground while inverted or everted).
Classification/Physical Exam
• Open (up to 25%) vs. Closed
• Medial: ~60-80% (Weatherford, Yoder 2011)
o Inversion injury
o Foot locked in plantar flexion and supinated (Menkes 2000)
o Sometimes referred to as “basketball foot”as it is seen when basketball players land after jumping) (Yoder 2011)
o Head of talus prominent dorsolaterally
• Lateral
o Eversion injury
o Foot locked in pronation
o Because of surrounding anatomical structures, lateral dislocation requires more force; thus, more frequently open and/or associated with other injuries (Yoder 2011)
o Calcaneus is displaced lateral to talus
• Anterior (from hyperextension) /Posterior (from hyperflexion)
o Much less common (< 5% of all dislocations) (DeLee 1982)
Diagnostic Imaging
• Dislocations will be clear on plain radiographs
• X-ray
o Obtain AP and lateral views of foot and ankle
o Medial Dislocation: talar head superior to navicular on lateral image
o Lateral Dislocation: talar head colinear or inferior to navicular bone on lateral image, non-distinguishable subtalar joint.(see figure 7)
ED Management
• Complete a primary and secondary trauma survey looking for additional injuries
• Assess neurovascular status and perform skin exam
• Provide analgesia
• Consider early consultation with orthopedics
o These dislocations are often much more difficult to reduce than standard ankle dislocations (tibio-talar dislocations)
o Up to 32% of subtalar dislocations require open reduction (Bibbo 2003)
Medial reduction can be blocked by capsule of talonavicular joint and extensor digitorum brevis, deep peroneal neurovascular bundle, talar head can “buttonhole” through the extensor digitorum brevis, or impaction can occur on navicular
Lateral reduction can be blocked by posterior tibial tendon (most common), impaction fractures, or other tendons
• Reduction Approach
o Standard ankle reduction techniques can lead to further injury and morbidity
o Flex the patient’s knee (90 degrees) and hip to reduce tension on the gastrocnemius and hold counter-traction (you may require an assistant for this)
o Place the ankle in plantar flexion
o For MEDIAL dislocations, grasp calcaneus with dominant hand, dorsum of foot with opposite hand, for LATERAL dislocations, do the same but also place non-dominant thumb over navicular
o Distract the hindfoot and apply direct pressure to talar head while inverting vs. everting to exaggerate the deformity
If patient is inverted (medial dislocation), hyper-invert
If patient is inverted everted (lateral dislocation), hyper-evert
Subsequently reverse the direction of dislocation (Thompson 2011)
• Post-Reduction
o Post-reduction X-rays
Confirm proper alignment
Evaluate for osteochondral lesions (injuries and/or small fractures of cartilage surface of talus), compression fractures, and other injuries of ankle/foot
o Consider post-reduction CT scan (Yoder 2011, Bibbo 2003)
Concomitant foot/ankle injuries are common (88-100%)
These injuries may be missed on plain radiographs
CT findings may change management and may affect outcomes
Optimal time to obtain CT scan (ED vs as outpatient) is unknown
o Short leg cast, non-weight bearing for 3-6 weeks (may consider short leg posterior/AO splint in ED after reduction for presumed swelling with close ortho follow up to transition to cast) (DeLee JC 1982)
Complications
o Post-Traumatic Arthritis
o Small number of subtalar fusions
o Lateral dislocations typically fare worse (as above, higher-energy mechanism, more frequent concomitant injuries)
o Infection with open wounds
* watch this video Subtalar Dislocation - Everything You Need To Know - Dr. Nabil Ebraheim
(see video 3)

Reference
• LAWRENCE E. WINESKI, PhD,Snell’s Clinical Anatomy by Regions, TENTH
• EDITION,1415-1416.
• Subtalar joint, teachmeanatomy,Stuart Jones, https://teachmeanatomy.info/lower-limb/joints/subtalar/
• Subtalar joint, Wikipedia, https://en.wikipedia.org/wiki/Subtalar_joint
• Subtalar joint, physio-pedia, https://www.physio-pedia.com/Subtalar_Joint
• Subtalar joint pain, southfloridasportsmedicine, http://www.southfloridasportsmedicine.com/subtalar.html
• Subtalar dislocation, coreem, https://coreem.net/core/subtalar-dislocation/
• EDITION,1415-1416.
• Subtalar joint, teachmeanatomy,Stuart Jones, https://teachmeanatomy.info/lower-limb/joints/subtalar/
• Subtalar joint, Wikipedia, https://en.wikipedia.org/wiki/Subtalar_joint
• Subtalar joint, physio-pedia, https://www.physio-pedia.com/Subtalar_Joint
• Subtalar joint pain, southfloridasportsmedicine, http://www.southfloridasportsmedicine.com/subtalar.html
• Subtalar dislocation, coreem, https://coreem.net/core/subtalar-dislocation/