The tibial nerve
By : Omair AlkatanOverview
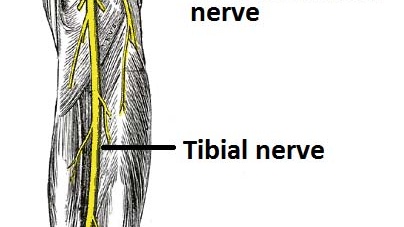
The tibial nerve is one of the 2 terminal branches of the sciatic nerve, the biggest nerve within the body. The tibial nerve originates from the L4-S3 spinal nerve roots and provides motor and sensory innervation to most of the posterior leg and foot. additionally to its motor branches, the branches of the tibial nerve include the medial sural cutaneous nerve, medial calcaneal nerve, and medial and lateral plantar nerves.
Function
Motor:
-Hip extension
-Knee flexion, internal rotation
-Ankle plantar flexion, inversion
-Hallux IP, MTP flexion
-Hallux abduction, adduction
-Second to fifth toe DIP, PIP, MTP flexion
-Second to fifth toe DIP, PIP extension (lumbricals, interossei)
-Second to fifth toe adduction, abduction
Sensory:
-Sensation to the posterolateral leg: medial sural -cutaneous nerve and sural nerve
-Sensation to the lateral side of the heel: sural nerve
-Sensation to the lateral surface of the foot: sural nerve
-Sensation to the medial side of the heel: medial calcaneal nerve
-Sensation to the lateral side of the plantar surface of the foot: lateral plantar nerve
-Sensation to the medial side of the plantar surface of the foot: medial plantar
-Hip extension
-Knee flexion, internal rotation
-Ankle plantar flexion, inversion
-Hallux IP, MTP flexion
-Hallux abduction, adduction
-Second to fifth toe DIP, PIP, MTP flexion
-Second to fifth toe DIP, PIP extension (lumbricals, interossei)
-Second to fifth toe adduction, abduction
Sensory:
-Sensation to the posterolateral leg: medial sural -cutaneous nerve and sural nerve
-Sensation to the lateral side of the heel: sural nerve
-Sensation to the lateral surface of the foot: sural nerve
-Sensation to the medial side of the heel: medial calcaneal nerve
-Sensation to the lateral side of the plantar surface of the foot: lateral plantar nerve
-Sensation to the medial side of the plantar surface of the foot: medial plantar
Path
To better perceive the tibial nerve and its functions, one would benefit from having an understanding of the nerve's course through the lower extremity, and a powerful grasp of the encompassing anatomy.
As expressed earlier, the tibial nerve may be a part of the sciatic nerve, the biggest nerve within the sciatic nerve. The nerve derives from the ventral rami of spinal nerves L4-S3, then exits the pelvis to some extent inferior to the piriformis muscle through the greater sciatic foramen to enter the posterior compartment of the thigh. whereas within the posterior thigh, it travels superficial to the adductor Magnus and deep to the biceps femoris, carrying fibers from the common peroneal and tibial nerves.
It is worth noting that there will be a major degree of anatomical variation seen with the sciatic nerve, and these variations cause several relevant clinical and surgical concerns. Tomaszewski et al. performed a meta-analysis of the nerve’s variations, examining a complete of 7210 lower limbs. the foremost common course of the sciatic nerve was as represented above: to exit the pelvis undivided directly below the piriformis muscle, and this pattern occurred in eighty-five. 2% of cases. however, in several cases, the sciatic nerve bifurcates into the tibial and common peroneal nerves inside the pelvis. In these cases, the tibial and common peroneal divisions of the sciatic nerve will pierce, exit above, or exit below the piriformis. an in-depth discussion of the variations of the sciatic nerve bifurcations is on the far side of the scope of this review. it's worth noting that piriformis syndrome happens once the sciatic nerve becomes entrapped in its course down the posterior leg. A bipartite piriformis and proximal division of the sciatic nerve are risk factors for this condition.
In cases wherever the sciatic nerve travels undivided through the posterior thigh, the nerve bifurcates a couple of centimeters superior to the popliteal fossa. The popliteal fossa is the area on the posterior side of the knee created by the border of 4 muscle bellies. Superomedially is the semimembranosus muscle, superolateral is the biceps femoris muscle, and inferomedially and inferolateral are the medial and lateral heads of the gastrocnemius, severally. From superficial to deep once viewed posteriorly, the popliteal fossa includes the tibial nerve, popliteal vein, saphenous vein, common peroneal nerve, and popliteal lymph nodes. The common peroneal nerve travels laterally once bifurcation, and it's usually visible within the superior border of the popliteal fossa close to the biceps femoris muscle. It continues laterally around the neck of the fibula to provide motor and sensory innervation to the leg.
The tibial nerve continues coursing inferiorly once its bifurcation and passes directly down the plane of the popliteal fossa to enter the leg. Before crossing the margin of any posterior leg muscles, the tibial nerve offers off its initial sensory branch: the medial sural cutaneous nerve. This nerve courses superficially between the 2 heads of the gastrocnemius muscle. It continues its course inferiorly close to the plane of the posterior leg to eventually unite with the sural communicating branch of the common fibular nerve.
Together, these nerves type the sural nerve, which continues coursing inferiorly to provide sensory innervation to the lateral side of the posterior leg.
The main trunk of the tibial nerve continues deep to the plantaris muscle and 2 heads of the gastrocnemius to enter the tendinous arch of the soleus muscle. currently, within the deep posterior compartment of the leg, the nerve continues its course on the posterior surface of the tibialis posterior muscle. It then passes simply posterior to the medial malleolus between the flexor digitorum longus and flexor hallucis longus among the tarsal tunnel. The calcaneus and talus bones form this tunnel on the deep/lateral side, and also the flexor retinaculum covers it superficially. The abductor hallucis forms the ground of this tunnel. From anterior to posterior, this tunnel contains the tibialis posterior tendon, flexor digitorum tendon, posterior tibial artery/vein, tibial nerve, and flexor hallucis longus tendon.
Just proximal to the tarsal tunnel, the tibial nerve offers off its second sensory branch, the medial calcaneal nerve. simply distal to the tarsal tunnel, the tibial nerve offers off its terminal branches, the medial and lateral plantar nerves, that still offer motor and sensory innervation to the plantar foot. These nerves travel within the second layer of the foot; the medial plantar nerve travels deep to the abductor hallucis to branch into the common plantar and eventually correct region digital nerves to the primary through fourth digits. The lateral plantar nerve travels obliquely to the lateral flexor of the foot deep to the skeletal muscle digitorum brevis and superficial to the quadratus Plantae muscle. This nerve then offers off a deep branch, that provides deep muscles of the foot, still as a superficial branch that continues coursing laterally. This superficial branch of the lateral plantar nerve terminates as common and correct region digital nerves supplying the fourth and fifth digits.
As expressed earlier, the tibial nerve may be a part of the sciatic nerve, the biggest nerve within the sciatic nerve. The nerve derives from the ventral rami of spinal nerves L4-S3, then exits the pelvis to some extent inferior to the piriformis muscle through the greater sciatic foramen to enter the posterior compartment of the thigh. whereas within the posterior thigh, it travels superficial to the adductor Magnus and deep to the biceps femoris, carrying fibers from the common peroneal and tibial nerves.
It is worth noting that there will be a major degree of anatomical variation seen with the sciatic nerve, and these variations cause several relevant clinical and surgical concerns. Tomaszewski et al. performed a meta-analysis of the nerve’s variations, examining a complete of 7210 lower limbs. the foremost common course of the sciatic nerve was as represented above: to exit the pelvis undivided directly below the piriformis muscle, and this pattern occurred in eighty-five. 2% of cases. however, in several cases, the sciatic nerve bifurcates into the tibial and common peroneal nerves inside the pelvis. In these cases, the tibial and common peroneal divisions of the sciatic nerve will pierce, exit above, or exit below the piriformis. an in-depth discussion of the variations of the sciatic nerve bifurcations is on the far side of the scope of this review. it's worth noting that piriformis syndrome happens once the sciatic nerve becomes entrapped in its course down the posterior leg. A bipartite piriformis and proximal division of the sciatic nerve are risk factors for this condition.
In cases wherever the sciatic nerve travels undivided through the posterior thigh, the nerve bifurcates a couple of centimeters superior to the popliteal fossa. The popliteal fossa is the area on the posterior side of the knee created by the border of 4 muscle bellies. Superomedially is the semimembranosus muscle, superolateral is the biceps femoris muscle, and inferomedially and inferolateral are the medial and lateral heads of the gastrocnemius, severally. From superficial to deep once viewed posteriorly, the popliteal fossa includes the tibial nerve, popliteal vein, saphenous vein, common peroneal nerve, and popliteal lymph nodes. The common peroneal nerve travels laterally once bifurcation, and it's usually visible within the superior border of the popliteal fossa close to the biceps femoris muscle. It continues laterally around the neck of the fibula to provide motor and sensory innervation to the leg.
The tibial nerve continues coursing inferiorly once its bifurcation and passes directly down the plane of the popliteal fossa to enter the leg. Before crossing the margin of any posterior leg muscles, the tibial nerve offers off its initial sensory branch: the medial sural cutaneous nerve. This nerve courses superficially between the 2 heads of the gastrocnemius muscle. It continues its course inferiorly close to the plane of the posterior leg to eventually unite with the sural communicating branch of the common fibular nerve.
Together, these nerves type the sural nerve, which continues coursing inferiorly to provide sensory innervation to the lateral side of the posterior leg.
The main trunk of the tibial nerve continues deep to the plantaris muscle and 2 heads of the gastrocnemius to enter the tendinous arch of the soleus muscle. currently, within the deep posterior compartment of the leg, the nerve continues its course on the posterior surface of the tibialis posterior muscle. It then passes simply posterior to the medial malleolus between the flexor digitorum longus and flexor hallucis longus among the tarsal tunnel. The calcaneus and talus bones form this tunnel on the deep/lateral side, and also the flexor retinaculum covers it superficially. The abductor hallucis forms the ground of this tunnel. From anterior to posterior, this tunnel contains the tibialis posterior tendon, flexor digitorum tendon, posterior tibial artery/vein, tibial nerve, and flexor hallucis longus tendon.
Just proximal to the tarsal tunnel, the tibial nerve offers off its second sensory branch, the medial calcaneal nerve. simply distal to the tarsal tunnel, the tibial nerve offers off its terminal branches, the medial and lateral plantar nerves, that still offer motor and sensory innervation to the plantar foot. These nerves travel within the second layer of the foot; the medial plantar nerve travels deep to the abductor hallucis to branch into the common plantar and eventually correct region digital nerves to the primary through fourth digits. The lateral plantar nerve travels obliquely to the lateral flexor of the foot deep to the skeletal muscle digitorum brevis and superficial to the quadratus Plantae muscle. This nerve then offers off a deep branch, that provides deep muscles of the foot, still as a superficial branch that continues coursing laterally. This superficial branch of the lateral plantar nerve terminates as common and correct region digital nerves supplying the fourth and fifth digits.
Posterior thigh compartment :
Semitendinosus
Origin: Ischial tuberosity
Insertion: Superior aspect of the medial surface of the tibia (pes anserinus)
Actions: Flexes knee, extends hip
Semimembranosus
Origin: Ischial tuberosity
Insertion: Posterior side of the medial condyle of the tibia
Actions: Flexes knee, extends hip
Biceps femoris long head
Origin: Ischial tuberosity
Insertion: Lateral side of the top of the fibula
Actions: Flexes knee, laterally rotates knee, extends hip
Adductor Magnus hamstring portion (vertical fibers)
Origin: Ischial tuberosity
Insertion: adductor tubercle of femur
Actions: Extends hip (vertical fibers)
Note: The adductor Magnus horizontal fibers receive innervation from the obturator nerve and contribute to the adduction and flexion of the hip
Superficial posterior leg compartment :
Gastrocnemius
Origin of lateral head: Lateral facet of lateral condyle of the femur
Origin of medial head: popliteal surface superior to the medial condyle of the femur
Insertion: Posterior aspect of the calcaneus (Achilles/calcaneal tendon)
Actions: plantar flexes ankle, flexes knee
Soleus
Origin: Posterior side of the top of the fibula, the proximal side of the posterior fibula, soleal line of the tibia
Insertion: Posterior side of the calcaneus (Achilles/calcaneal tendon)
Actions: plantar flexes the ankle
Plantaris
Origin: Lateral supracondylar line of the femur, oblique popliteal ligament
Insertion: Posterior side of the calcaneus (Achilles/calcaneal tendon)
Actions: region flexes plantar (weak), flexes knee (weak)
Deep posterior leg compartment :
Popliteus
Origin: Lateral side of the lateral femoral condyle, lateral meniscus
Insertion: Posterior tibia superior to soleal line
Actions: Internally rotates knee (unlocks knee), flexes knee (weak)
Tibialis posterior
Origin: Posterior tibia inferior to the soleal line, interosseous membrane, the proximal side of the posterior fibula
Insertion: tuberosity of navicular bone, medial, intermediate, lateral four cuneiforms, cuboid, the bottom of the second through the fourth metatarsal
Actions: plantar flexes ankle, inverts ankle joint
Flexor digitorum longus
Origin: Medial side of posterior tibia inferior to the soleal line
Insertion: Base of the second through fifth distal phalanges
Actions: Flexes second through fifth DIP, PIP, MTP, plantar flexes ankle
Flexor hallucis longus
Origin: Distal side of the posterior fibula, interosseous membrane
Insertion: Base of hallux distal phalanx
Actions: Flexes hallux IP, MTP, plantar flexes ankle (weak)
Medial plantar branch :
Abductor hallucis
Origin: tuberosity of calcaneus, plantar aponeurosis
Insertion: Medial side of the bottom of hallux proximal phalanx
Actions: Abducts hallux, flexes hallux MTP
Flexor digitorum brevis
Origin: tuberosity of calcaneus, plantar aponeurosis
Insertion: Second through fifth middle phalanges
Actions: Flexes second through fifth PIP, MTP
Flexor hallucis brevis
Origin: plantar side of the cuboid, plantar side of lateral cuneiform
Insertion: Base of hallux proximal phalanx
Actions: Flexes hallux MTP
1st lumbrical (not named in reference to digits)
Origin: tendon of flexor digitorum longus
Insertion: Medial side of the second phalanx extensor expansion
Actions: Flexes second MTP, extends second DIP, PIP
Lateral plantar branch:
Quadratus Plantae
Origin: Medial and lateral aspects of the plantar surface of the calcaneus
Insertion: flexor digitorum longus tendon (posterolateral aspect)
Actions: Assists in flexor digitorum longus flexion by correcting for its obliquely directed contraction
Abductor digiti minimi
Origin: tuberosity of calcaneus, plantar aponeurosis
Insertion: Lateral side of the base of the fifth proximal phalanx
Actions: Abducts fifth phalanx, flexes fifth MTP
Flexor digiti minimi brevis
Origin: Base of the fifth metatarsal
Insertion: Lateral side of the bottom of the fifth proximal phalanx
Actions: Flexes fifth MTP
First through third plantar interossei (not named in reference to digits)
Origination: Medial surface and base of third through fifth metatarsals
Insertion: Medial facet of third through fifth proximal phalanges
Actions: Adducts third through fifth phalanges, flexes third through fifth MTP
First through fourth dorsal interossei (not named in reference to digits)
Origin: Adjacent aspects of initial through fifth metatarsals
Insertion of initial dorsal interossei: Medial side of the second proximal phalanx
Insertion of the second through fourth dorsal interossei: Lateral side of second through fourth proximal phalanx, tendons of extensor digitorum longus
Action: Abducts third and fourth phalanges, flexes second through the fourth MTP, extends second through fourth DIP, PIP
Opposing action of initial and second dorsal interossei on the second phalanx results in no abduction of the second phalanx
Second through fourth lumbricals (not named in reference to digits)
Origin: Tendons of flexor digitorum longus
Insertion: Medial side of third through fifth phalanx extensor expansion
Actions: Flexes third through fifth MTP, extends third through fifth DIP, PIP
Adductor hallucis
Origin of oblique head: Base of second through fourth metatarsals
Origin of transverse head: Third through fifth MTP ligaments
Insertion: Lateral side of hallux proximal phalanx
Actions: Adducts hallux
As with any nerve, harm will occur through direct trauma or induced injury. Specific to the tibial nerve, however, are 2 conditions of interest.
Tarsal Tunnel Syndrome
Tarsal tunnel syndrome results from tibial nerve compression inside the tarsal tunnel, quite analogous to the more well-known carpal tunnel syndrome of the wrist. once coursing inferomedially inside the leg, the tibial nerve enters the foot through the tarsal tunnel. This compartment is fairly slim at baseline, therefore any etiology of increased pressure in this region will cause compression of the tibial nerve. Etiologies are typically broken down into intrinsic and extrinsic sources. Intrinsic causes include abnormal growths (ganglion cysts, osteophytes, osteochondromas, schwannomas), peri-neural fibrosis, and hypertrophic tendinopathies. extrinsic causes include trauma (ankle sprains, post-surgical scarring), edema, obesity, and tight shoes.
Patients typically present with burning, numbness, or tingling within the plantar surface of the foot and toes. Symptoms may additionally be experienced in the heel through radiation to the medial calcaneal nerve, that branches proximal to the tarsal tunnel. The pain is usually most pronounced with prolonged standing and manual pressure over the medial aspect of the gliding joint. Tinel sign, which is tingling upon percussion of the nerve, is positive in additional than 1/2 of patients. In severe cases, patients might experience muscle weakness and muscle wasting.
Management includes lifestyle modifications for extrinsic causes (weight loss, change of shoes), and initial conservative treatment for different cases. This includes resting of the foot and ankle, and potential use of corticosteroid injections. it's suggested that conservative treatment is tried for 6 months before going to surgery unless the case is because of direct trauma or previous surgery. Surgical management involves decompression of the tibial nerve, which frequently involves the manipulation of the flexor retinaculum and fascia of the abductor hallucis brevis.
Compartment Syndrome
Many muscle groups within the human extremities are engulfed in fascial membranes. In the leg, there are four fascial envelopes or compartments: anterior, lateral, superficial posterior, and deep posterior. Compartment syndrome is represented as an acute or chronic increase in pressure inside a fascial compartment that results in a compromise of the blood provide to structures inside the compartment. Anterior compartment syndrome is the most typical of those four, however, every one of the four compartments will be involved. Compartment syndromes occur most typically the following trauma because of progressive limb swelling that will increase pressure within the compartment leading to blood vessel hypertension and eventual tissue anemia.
Untreated compartment syndrome of the deep posterior compartment may result in motor and sensory deficits within the foot and ankle because of tibial nerve ischemia. Deficits include paresthesias of the plantar foot and weakness within the toe and plantar flexion. Fasciotomy, which involves an incision within the encompassing fascia resulting in reduced pressure inside the compartment, is the primary technique of treatment in symptomatic patients. In acute cases, immediate decompression is critical to avoid irreversible tissue death.
Semitendinosus
Origin: Ischial tuberosity
Insertion: Superior aspect of the medial surface of the tibia (pes anserinus)
Actions: Flexes knee, extends hip
Semimembranosus
Origin: Ischial tuberosity
Insertion: Posterior side of the medial condyle of the tibia
Actions: Flexes knee, extends hip
Biceps femoris long head
Origin: Ischial tuberosity
Insertion: Lateral side of the top of the fibula
Actions: Flexes knee, laterally rotates knee, extends hip
Adductor Magnus hamstring portion (vertical fibers)
Origin: Ischial tuberosity
Insertion: adductor tubercle of femur
Actions: Extends hip (vertical fibers)
Note: The adductor Magnus horizontal fibers receive innervation from the obturator nerve and contribute to the adduction and flexion of the hip
Superficial posterior leg compartment :
Gastrocnemius
Origin of lateral head: Lateral facet of lateral condyle of the femur
Origin of medial head: popliteal surface superior to the medial condyle of the femur
Insertion: Posterior aspect of the calcaneus (Achilles/calcaneal tendon)
Actions: plantar flexes ankle, flexes knee
Soleus
Origin: Posterior side of the top of the fibula, the proximal side of the posterior fibula, soleal line of the tibia
Insertion: Posterior side of the calcaneus (Achilles/calcaneal tendon)
Actions: plantar flexes the ankle
Plantaris
Origin: Lateral supracondylar line of the femur, oblique popliteal ligament
Insertion: Posterior side of the calcaneus (Achilles/calcaneal tendon)
Actions: region flexes plantar (weak), flexes knee (weak)
Deep posterior leg compartment :
Popliteus
Origin: Lateral side of the lateral femoral condyle, lateral meniscus
Insertion: Posterior tibia superior to soleal line
Actions: Internally rotates knee (unlocks knee), flexes knee (weak)
Tibialis posterior
Origin: Posterior tibia inferior to the soleal line, interosseous membrane, the proximal side of the posterior fibula
Insertion: tuberosity of navicular bone, medial, intermediate, lateral four cuneiforms, cuboid, the bottom of the second through the fourth metatarsal
Actions: plantar flexes ankle, inverts ankle joint
Flexor digitorum longus
Origin: Medial side of posterior tibia inferior to the soleal line
Insertion: Base of the second through fifth distal phalanges
Actions: Flexes second through fifth DIP, PIP, MTP, plantar flexes ankle
Flexor hallucis longus
Origin: Distal side of the posterior fibula, interosseous membrane
Insertion: Base of hallux distal phalanx
Actions: Flexes hallux IP, MTP, plantar flexes ankle (weak)
Medial plantar branch :
Abductor hallucis
Origin: tuberosity of calcaneus, plantar aponeurosis
Insertion: Medial side of the bottom of hallux proximal phalanx
Actions: Abducts hallux, flexes hallux MTP
Flexor digitorum brevis
Origin: tuberosity of calcaneus, plantar aponeurosis
Insertion: Second through fifth middle phalanges
Actions: Flexes second through fifth PIP, MTP
Flexor hallucis brevis
Origin: plantar side of the cuboid, plantar side of lateral cuneiform
Insertion: Base of hallux proximal phalanx
Actions: Flexes hallux MTP
1st lumbrical (not named in reference to digits)
Origin: tendon of flexor digitorum longus
Insertion: Medial side of the second phalanx extensor expansion
Actions: Flexes second MTP, extends second DIP, PIP
Lateral plantar branch:
Quadratus Plantae
Origin: Medial and lateral aspects of the plantar surface of the calcaneus
Insertion: flexor digitorum longus tendon (posterolateral aspect)
Actions: Assists in flexor digitorum longus flexion by correcting for its obliquely directed contraction
Abductor digiti minimi
Origin: tuberosity of calcaneus, plantar aponeurosis
Insertion: Lateral side of the base of the fifth proximal phalanx
Actions: Abducts fifth phalanx, flexes fifth MTP
Flexor digiti minimi brevis
Origin: Base of the fifth metatarsal
Insertion: Lateral side of the bottom of the fifth proximal phalanx
Actions: Flexes fifth MTP
First through third plantar interossei (not named in reference to digits)
Origination: Medial surface and base of third through fifth metatarsals
Insertion: Medial facet of third through fifth proximal phalanges
Actions: Adducts third through fifth phalanges, flexes third through fifth MTP
First through fourth dorsal interossei (not named in reference to digits)
Origin: Adjacent aspects of initial through fifth metatarsals
Insertion of initial dorsal interossei: Medial side of the second proximal phalanx
Insertion of the second through fourth dorsal interossei: Lateral side of second through fourth proximal phalanx, tendons of extensor digitorum longus
Action: Abducts third and fourth phalanges, flexes second through the fourth MTP, extends second through fourth DIP, PIP
Opposing action of initial and second dorsal interossei on the second phalanx results in no abduction of the second phalanx
Second through fourth lumbricals (not named in reference to digits)
Origin: Tendons of flexor digitorum longus
Insertion: Medial side of third through fifth phalanx extensor expansion
Actions: Flexes third through fifth MTP, extends third through fifth DIP, PIP
Adductor hallucis
Origin of oblique head: Base of second through fourth metatarsals
Origin of transverse head: Third through fifth MTP ligaments
Insertion: Lateral side of hallux proximal phalanx
Actions: Adducts hallux
As with any nerve, harm will occur through direct trauma or induced injury. Specific to the tibial nerve, however, are 2 conditions of interest.
Tarsal Tunnel Syndrome
Tarsal tunnel syndrome results from tibial nerve compression inside the tarsal tunnel, quite analogous to the more well-known carpal tunnel syndrome of the wrist. once coursing inferomedially inside the leg, the tibial nerve enters the foot through the tarsal tunnel. This compartment is fairly slim at baseline, therefore any etiology of increased pressure in this region will cause compression of the tibial nerve. Etiologies are typically broken down into intrinsic and extrinsic sources. Intrinsic causes include abnormal growths (ganglion cysts, osteophytes, osteochondromas, schwannomas), peri-neural fibrosis, and hypertrophic tendinopathies. extrinsic causes include trauma (ankle sprains, post-surgical scarring), edema, obesity, and tight shoes.
Patients typically present with burning, numbness, or tingling within the plantar surface of the foot and toes. Symptoms may additionally be experienced in the heel through radiation to the medial calcaneal nerve, that branches proximal to the tarsal tunnel. The pain is usually most pronounced with prolonged standing and manual pressure over the medial aspect of the gliding joint. Tinel sign, which is tingling upon percussion of the nerve, is positive in additional than 1/2 of patients. In severe cases, patients might experience muscle weakness and muscle wasting.
Management includes lifestyle modifications for extrinsic causes (weight loss, change of shoes), and initial conservative treatment for different cases. This includes resting of the foot and ankle, and potential use of corticosteroid injections. it's suggested that conservative treatment is tried for 6 months before going to surgery unless the case is because of direct trauma or previous surgery. Surgical management involves decompression of the tibial nerve, which frequently involves the manipulation of the flexor retinaculum and fascia of the abductor hallucis brevis.
Compartment Syndrome
Many muscle groups within the human extremities are engulfed in fascial membranes. In the leg, there are four fascial envelopes or compartments: anterior, lateral, superficial posterior, and deep posterior. Compartment syndrome is represented as an acute or chronic increase in pressure inside a fascial compartment that results in a compromise of the blood provide to structures inside the compartment. Anterior compartment syndrome is the most typical of those four, however, every one of the four compartments will be involved. Compartment syndromes occur most typically the following trauma because of progressive limb swelling that will increase pressure within the compartment leading to blood vessel hypertension and eventual tissue anemia.
Untreated compartment syndrome of the deep posterior compartment may result in motor and sensory deficits within the foot and ankle because of tibial nerve ischemia. Deficits include paresthesias of the plantar foot and weakness within the toe and plantar flexion. Fasciotomy, which involves an incision within the encompassing fascia resulting in reduced pressure inside the compartment, is the primary technique of treatment in symptomatic patients. In acute cases, immediate decompression is critical to avoid irreversible tissue death.
References
1-Tomaszewski KA, Graves MJ, Henry BM, Popieluszko P, Roy J, Pękala PA, Hsieh WC, Vikse J, Walocha JA. Surgical anatomy of the sciatic nerve: A meta-analysis. J Orthop Res. 2016 Oct;34(10):1820-1827. [PubMed]
2-Hicks BL, Lam JC, Varacallo M. StatPearls [Internet]. StatPearls Publishing; Treasure Island (FL): Jul 18, 2021. Piriformis Syndrome. [PubMed]
3-Iida T, Kobayashi M. Tibial nerve entrapment at the tendinous arch of the soleus: a case report. Clin Orthop Relat Res. 1997 Jan;(334):265-9. [PubMed]
4-Day CP, Orme R. Popliteal artery branching patterns -- an angiographic study. Clin Radiol. 2006 Aug;61(8):696-9. [PubMed]
5-Ransom AL, Sinkler MA, Nallamothu SV. StatPearls [Internet]. StatPearls Publishing; Treasure Island (FL): Oct 6, 2021. Anatomy, Bony Pelvis and Lower Limb, Femoral Muscles. [PubMed]
6-Binstead JT, Munjal A, Varacallo M. StatPearls [Internet]. StatPearls Publishing; Treasure Island (FL): Jun 3, 2021. Anatomy, Bony Pelvis and Lower Limb, Calf. [PubMed]
7-Bourne M, Sinkler MA, Murphy PB. StatPearls [Internet]. StatPearls Publishing; Treasure Island (FL): Aug 11, 2021. Anatomy, Bony Pelvis and Lower Limb, Tibia. [PubMed]
8-Kalin PJ, Hirsch BE. The origins and function of the interosseous muscles of the foot. J Anat. 1987 Jun;152:83-91. [PMC free article] [PubMed]
9-Faucett SC, Gannon J, Chahla J, Ferrari MB, LaPrade RF. Posterior Surgical Approach to the Knee. Arthrosc Tech. 2017 Apr;6(2):e391-e395. [PMC free article] [PubMed]
10-Acevedo JI, Busch MT, Ganey TM, Hutton WC, Ogden JA. Coaxial portals for posterior ankle arthroscopy: An anatomic study with clinical correlation on 29 patients. Arthroscopy. 2000 Nov;16(8):836-42. [PubMed]
11- image contributed from teachmeanatomy site