Interosseous Membrane Of Forearm
By : Najah SabahDefinition
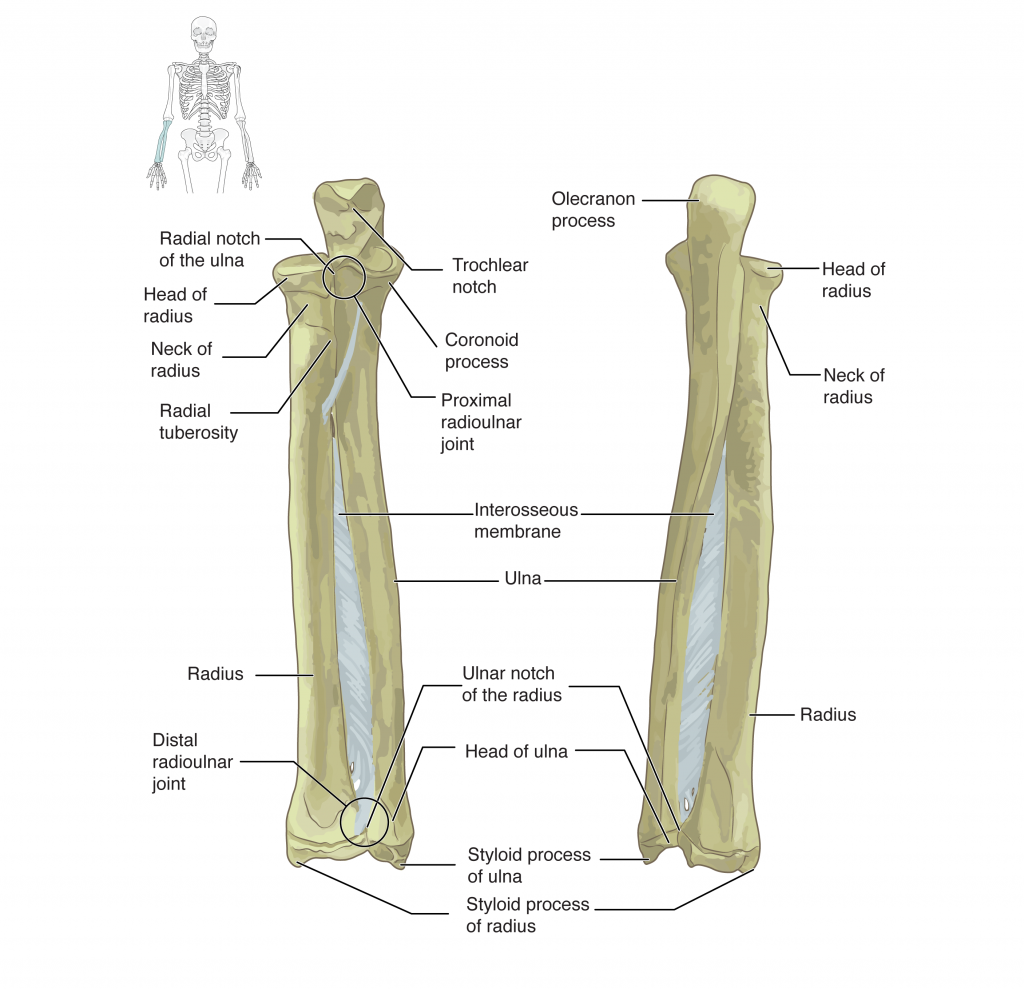
the interosseous membrane is a fibrous tissue with an oblique orientation from the radius to the ulna. The membrane maintains the interosseous space between the radius and ulna through forearm rotation and actively transfers forces from the radius to the ulna.(see figure 1)
FUNCTION
The interosseous membrane divides the forearm into anterior and posterior compartments, serves as a site of attachment for muscles of the forearm, and transfers loads placed on the forearm.
The interosseous membrane is designed to shift compressive loads (as in doing a hand-stand) from the distal radius to the proximal ulna. The fibers within the interosseous membrane are oriented obliquely so that when force is applied the fibers are drawn taut, shifting more of the load to the ulna. This reduces the wear and tear of placing the whole load on a single joint. The role of the membrane in load shifting is illustrated when the interosseous membrane is cut; the forces on each bone equalize from their natural proportions.
Additionally, as the forearm moves from pronation to supination, the interosseous membrane fibers change from a relaxed state, to a tense state in the neutral position. They once again become relaxed as the forearm enters pronation.
The interosseous membrane is designed to shift compressive loads (as in doing a hand-stand) from the distal radius to the proximal ulna. The fibers within the interosseous membrane are oriented obliquely so that when force is applied the fibers are drawn taut, shifting more of the load to the ulna. This reduces the wear and tear of placing the whole load on a single joint. The role of the membrane in load shifting is illustrated when the interosseous membrane is cut; the forces on each bone equalize from their natural proportions.
Additionally, as the forearm moves from pronation to supination, the interosseous membrane fibers change from a relaxed state, to a tense state in the neutral position. They once again become relaxed as the forearm enters pronation.
The interosseous membrane is composed of five ligaments
1. - Central band (key portion to be reconstructed in case of injury)
2. - Accessory band
3. - Distal oblique bundle
4. - Proximal oblique cord
5. - Dorsal oblique accessory cor d
(see figure 2)
2. - Accessory band
3. - Distal oblique bundle
4. - Proximal oblique cord
5. - Dorsal oblique accessory cor d
(see figure 2)

The structures related to it :
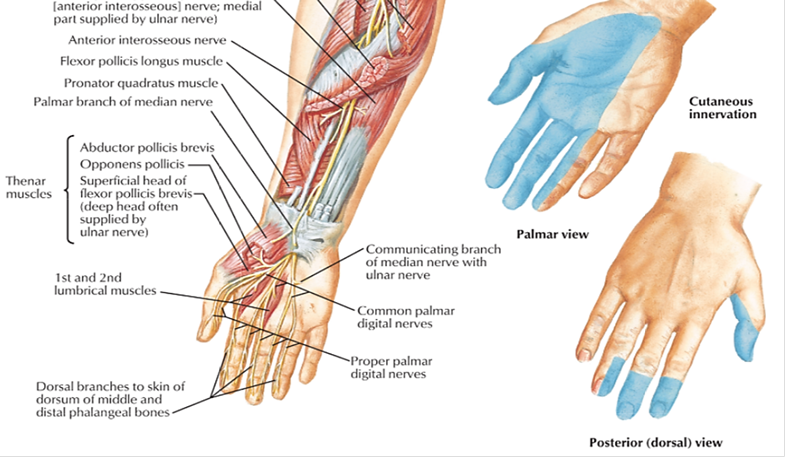
1. Anterior interosseous nerve : the deep division of median nerve which supplies muscles of anterior compartment of forearm .
2. Anterior interosseous artery : branch of ulnar artery.
3. Posterior interosseous nerve : the deep division of radial nerve which supplies muscles of posterior compartment of forearm.
4. Posterior interosseous artery : branch of ulnar artery.
5. Common interosseous artery : terminal branch of ulnar artery.
6. Recurrent interosseous artery : branch of ulnar artery which shares in the anastomosis around the elbow joint.
(see figure 3)
2. Anterior interosseous artery : branch of ulnar artery.
3. Posterior interosseous nerve : the deep division of radial nerve which supplies muscles of posterior compartment of forearm.
4. Posterior interosseous artery : branch of ulnar artery.
5. Common interosseous artery : terminal branch of ulnar artery.
6. Recurrent interosseous artery : branch of ulnar artery which shares in the anastomosis around the elbow joint.
(see figure 3)


Related structures
Injury
Severe forearm injuries involving separation of the radius and ulna may be due to rupture of the interosseous membrane. Rupture can lead to proximal migration of the radius and an apparent lengthening of the ulna at the wrist. Often interosseous membrane tears are associated with adverse impacts on forearm rotation. MRI-assisted diagnosis has been used for mid-substance tears of the interosseous membrane but is expensive and not widely available. On the contrary, ultrasound has proven useful in diagnosing tears of the tibiofibular interosseous membrane of the leg, and this technique may also be applied to acute cases of membrane tears in the forearm due to its low cost and portability.
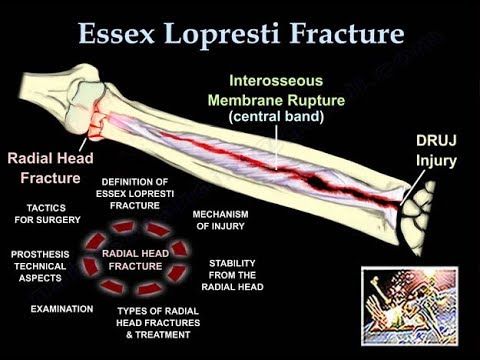
Injury of interosseous membrane of forearm : Essex-Lopresti injury
Other Names
• Essex Lopresti fracture-dislocation
• Essex-Lopresti Injury
• Longitudinal Radioulnar Dissociation
________________________________________
The Essex Lopresti injury affects the axial stability of the forearm. It is an injury to the interosseous membrane and the triangular fibrocartilage complex which could result in proximal migration of the radius. The Essex Lopresti fractures is difficult to diagnose, and the physician must restore the stability of the elbow and the DRUJ.
The mechanism of injury is usually a fall onto an outstretched hand. The elbow will be in extension and pronation. There will be axial loading transmitted from the wrist to the radial head, which is combined with a valgus force, and this will create a fracture of the radial head. The radial head provides two types of stability: valgus stability and longitudinal stability. The radial head is secondary restraint to valgus load at the elbow, and it prevents proximal migration of the radius with some contribution from the interosseous membrane. Loss of this longitudinal stability occurs when the radial head fractures, plus injury to the DRUJ, and the interosseous membrane will become ruptured in this situation. In this situation, the radial head should be fixed or if the radial head is unreconstructable, replace the radial had by a radial head prosthesis, but never resect the radial head alone in this situation without replacing it. Radial head excision will result in proximal migration of the radius and ulnocarpal impingement with distal radioulnar joint instability. The problem is that not all hospitals are equipped with radial head prosthesis. You can excise the radial head if all ligaments are intact, but the problem is that you may not know that the DRUJ is involved.
There are four types of radial head fractures:
1-Type I is a nondisplaced fracture which has no block to forearm rotation. It has an early range of motion and does not require surgical treatment.
2- Type II is a displaced fracture more than 2 mm. it requires fixation by screws or a plate.
3-Type III is a comminuted fracture that is displaced or irreparable. It requires excision and prosthesis typically a metallic modular prosthesis. Excision alone can be done in some situations. Before you excise the radial head fracture, you must make sure all ligaments are intact, that you examined the patient and that there is no distal radioulnar joint (DRUJ) injury or elbow injury. If you have a patient with a comminuted radial head fracture, it is probably safer to replace it.
4-Type IV fractures are associated with dislocation of the elbow joint. You should attempt to reduce the elbow joint with fixation of the fracture. This can be done with a plate or screws. Excision of the radial head and prosthetic replacement if the fracture is unreconstructable (cannot be repaired). Excision of the radial head alone is contraindicated in elbow dislocation or in Essex Lopresti fracture.
To examine Essex Lopresti Fractures : you must first examine the DRUJ: Palpate the wrist for tenderness and excessive translation of the DRUJ. Examination of the DRUJ is very difficult; be sure to check the x-rays carefully. You may want to do the squeeze test, similar to what you do to check for high syndesmotic injury of the ankle and check if there is any tenderness there. You may want to get dynamic CT scans before surgery (it may show you some instability at the DRUJ. In surgery, you will do the radius pull test. More than 3mm of translation is concerning for longitudinal forearm instability (Lum & Trzeciak, 2018).
Surgical treatment :
Surgery for radial head fractures is done through posterolateral (Kocher) approach between the ECU and Anconeus muscles or through the lateral approach. Watch the safe zone for implant insertion to avoid impingement and loss of rotation. The radial head prosthesis usually I s cementless and acts as a stiff spacer until the ligaments heal, so it doesn’t have to be very snug into the canal (may fracture the proximal radius). You can use the modular system to check for the appropriate height. Make sure that you do not over stuff it. Visually assess widening of the lateral ulnohumeral joint, and also make sure that you are not blocking extension. You want to keep the lateral ulnar collateral ligament (ulnar humeral ligament) intact and stay above the equator of the radial head. When you stay above the equator in the radial head, it is less likely that you will injure the lateral ulnar collateral ligament (LUCL). Make sure that you understand the position of the posterior interosseous nerve which is about 4 cm. the posterior interosseous nerve crosses the proximal radius from anteriorly to posteriorly within the supinator muscle, 4 cm distal to the radial head. When you do the surgery, you want to pronate the forearm to protect the posterior interosseous nerve. Pronation pulls the nerve anteriorly away from the surgical field.
(see figure 4)(see video below)
• Essex Lopresti fracture-dislocation
• Essex-Lopresti Injury
• Longitudinal Radioulnar Dissociation
________________________________________
The Essex Lopresti injury affects the axial stability of the forearm. It is an injury to the interosseous membrane and the triangular fibrocartilage complex which could result in proximal migration of the radius. The Essex Lopresti fractures is difficult to diagnose, and the physician must restore the stability of the elbow and the DRUJ.
The mechanism of injury is usually a fall onto an outstretched hand. The elbow will be in extension and pronation. There will be axial loading transmitted from the wrist to the radial head, which is combined with a valgus force, and this will create a fracture of the radial head. The radial head provides two types of stability: valgus stability and longitudinal stability. The radial head is secondary restraint to valgus load at the elbow, and it prevents proximal migration of the radius with some contribution from the interosseous membrane. Loss of this longitudinal stability occurs when the radial head fractures, plus injury to the DRUJ, and the interosseous membrane will become ruptured in this situation. In this situation, the radial head should be fixed or if the radial head is unreconstructable, replace the radial had by a radial head prosthesis, but never resect the radial head alone in this situation without replacing it. Radial head excision will result in proximal migration of the radius and ulnocarpal impingement with distal radioulnar joint instability. The problem is that not all hospitals are equipped with radial head prosthesis. You can excise the radial head if all ligaments are intact, but the problem is that you may not know that the DRUJ is involved.
There are four types of radial head fractures:
1-Type I is a nondisplaced fracture which has no block to forearm rotation. It has an early range of motion and does not require surgical treatment.
2- Type II is a displaced fracture more than 2 mm. it requires fixation by screws or a plate.
3-Type III is a comminuted fracture that is displaced or irreparable. It requires excision and prosthesis typically a metallic modular prosthesis. Excision alone can be done in some situations. Before you excise the radial head fracture, you must make sure all ligaments are intact, that you examined the patient and that there is no distal radioulnar joint (DRUJ) injury or elbow injury. If you have a patient with a comminuted radial head fracture, it is probably safer to replace it.
4-Type IV fractures are associated with dislocation of the elbow joint. You should attempt to reduce the elbow joint with fixation of the fracture. This can be done with a plate or screws. Excision of the radial head and prosthetic replacement if the fracture is unreconstructable (cannot be repaired). Excision of the radial head alone is contraindicated in elbow dislocation or in Essex Lopresti fracture.
To examine Essex Lopresti Fractures : you must first examine the DRUJ: Palpate the wrist for tenderness and excessive translation of the DRUJ. Examination of the DRUJ is very difficult; be sure to check the x-rays carefully. You may want to do the squeeze test, similar to what you do to check for high syndesmotic injury of the ankle and check if there is any tenderness there. You may want to get dynamic CT scans before surgery (it may show you some instability at the DRUJ. In surgery, you will do the radius pull test. More than 3mm of translation is concerning for longitudinal forearm instability (Lum & Trzeciak, 2018).
Surgical treatment :
Surgery for radial head fractures is done through posterolateral (Kocher) approach between the ECU and Anconeus muscles or through the lateral approach. Watch the safe zone for implant insertion to avoid impingement and loss of rotation. The radial head prosthesis usually I s cementless and acts as a stiff spacer until the ligaments heal, so it doesn’t have to be very snug into the canal (may fracture the proximal radius). You can use the modular system to check for the appropriate height. Make sure that you do not over stuff it. Visually assess widening of the lateral ulnohumeral joint, and also make sure that you are not blocking extension. You want to keep the lateral ulnar collateral ligament (ulnar humeral ligament) intact and stay above the equator of the radial head. When you stay above the equator in the radial head, it is less likely that you will injure the lateral ulnar collateral ligament (LUCL). Make sure that you understand the position of the posterior interosseous nerve which is about 4 cm. the posterior interosseous nerve crosses the proximal radius from anteriorly to posteriorly within the supinator muscle, 4 cm distal to the radial head. When you do the surgery, you want to pronate the forearm to protect the posterior interosseous nerve. Pronation pulls the nerve anteriorly away from the surgical field.
(see figure 4)(see video below)

Reference:
1. Saladin, Kenneth (2012). Anatomy and Physiology: The Unity of Form and Function 6th Edition. New York, NY: McGraw-Hill. p. 263. .
2. ^ Birkbeck, D. P.; Failla, J. M.; Hoshaw, S. J.; Fyhrie, D. P.; Schaffler, M. (1997-11-01). "The interosseous membrane affects load distribution in the forearm". The Journal of Hand Surgery. 22 (6): 975–980. ^ Wallace, A. L.; Walsh, W. R.; van Rooijen, M.; Hughes, J. S.; Sonnabend, D. H. (1997-05-01). "The interosseous membrane in radioulnar dissociation". The Journal of Bone and Joint Surgery. British Volume. 79 (3): 422–427
2. ^ Birkbeck, D. P.; Failla, J. M.; Hoshaw, S. J.; Fyhrie, D. P.; Schaffler, M. (1997-11-01). "The interosseous membrane affects load distribution in the forearm". The Journal of Hand Surgery. 22 (6): 975–980. ^ Wallace, A. L.; Walsh, W. R.; van Rooijen, M.; Hughes, J. S.; Sonnabend, D. H. (1997-05-01). "The interosseous membrane in radioulnar dissociation". The Journal of Bone and Joint Surgery. British Volume. 79 (3): 422–427