Joints Of The Leg
By : Najah Sabahcontents
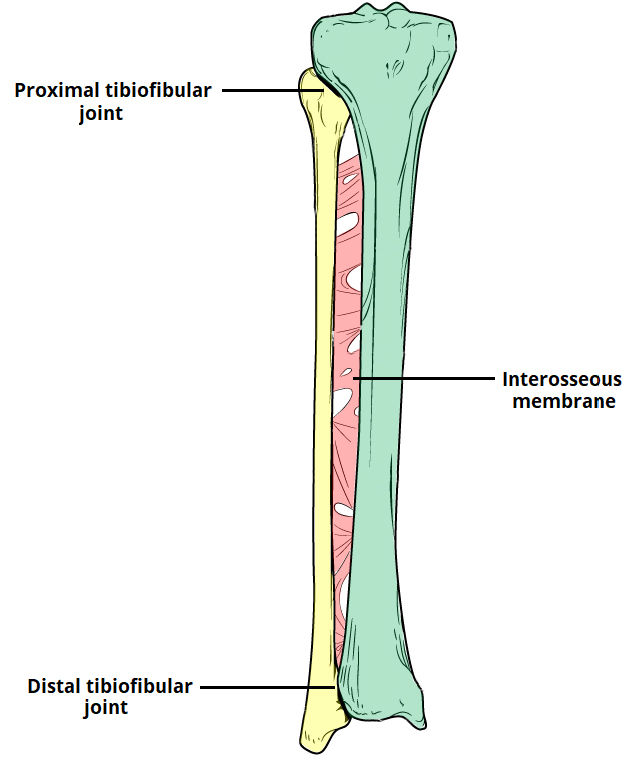
1. Proximal tibiofibular joint.
3. Distal tibiofibular joint (anterior&posterior).
2. Middle tibiofibular joint (interosseous membrane of the leg).
3. Distal tibiofibular joint (anterior&posterior).
2. Middle tibiofibular joint (interosseous membrane of the leg).
1-Proximal Tibiofibular Joint
Definition
Proximal Tibiofibular Joint
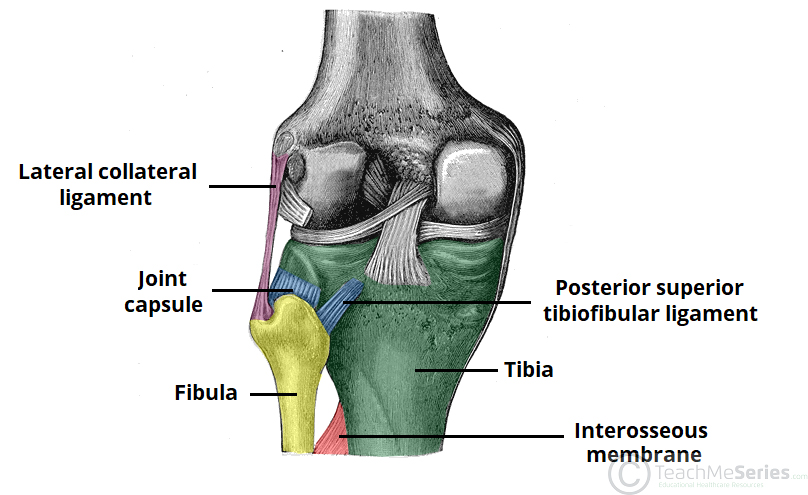
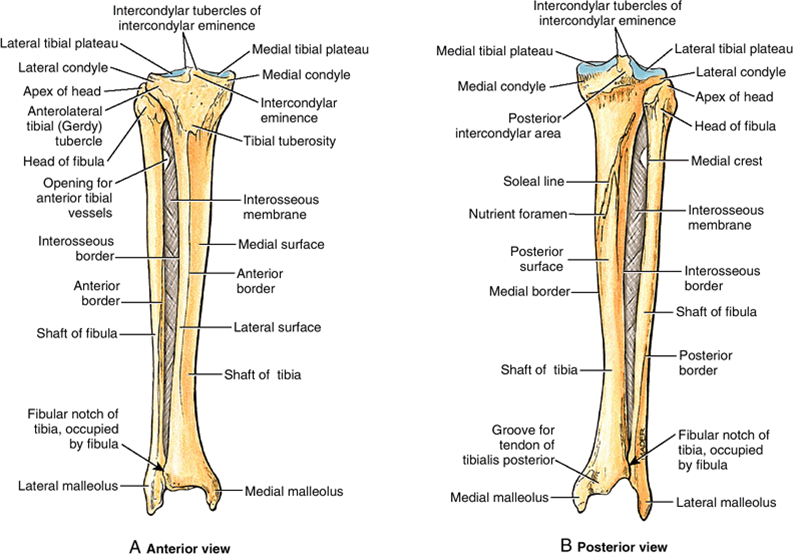
Articulation is between the lateral condyle of the tibia and the head of the fibula The articular surfaces are flattened and covered byhyaline cartilage.
(see figure 1)
Type
This is a synovial, plane, gliding joint.
Capsule
The capsule surrounds the joint and is attached to the margins of the articular surfaces.
Ligaments
Anterior and posterior ligaments strengthen the capsule. The interosseous membrane, which connects the shafts of the tibia and fibula together, also greatly strengthens the joint.( see figure 1)
Synovial Membrane
The synovial membrane lines the capsule and is attached to the margins othe articular surfaces.
Articulation is between the lateral condyle of the tibia and the head of the fibula The articular surfaces are flattened and covered byhyaline cartilage.
(see figure 1)
Type
This is a synovial, plane, gliding joint.
Capsule
The capsule surrounds the joint and is attached to the margins of the articular surfaces.
Ligaments
Anterior and posterior ligaments strengthen the capsule. The interosseous membrane, which connects the shafts of the tibia and fibula together, also greatly strengthens the joint.( see figure 1)
Synovial Membrane
The synovial membrane lines the capsule and is attached to the margins othe articular surfaces.
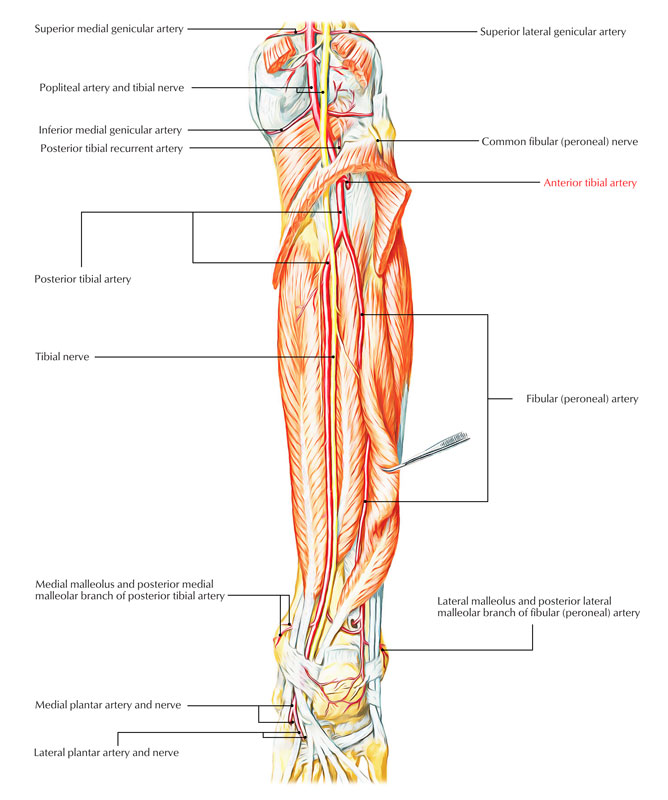
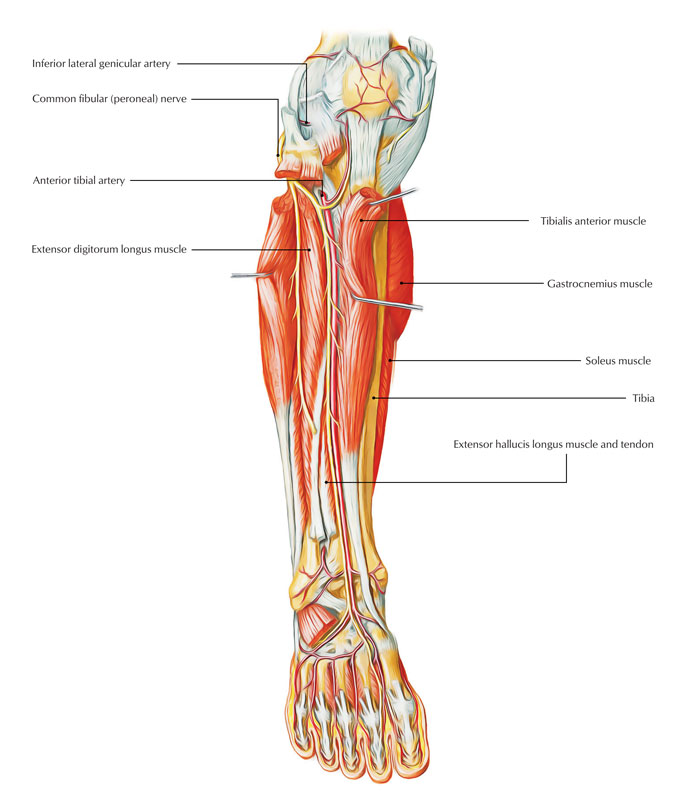
Vascular supply and lymphatic drainage
The superior tibiofibular joint receives an arterial supply from the anterior and posteriortibial recurrent branches of the anterior tibial artery. Lymphatics follow the arteries and drain to the popliteal nodes.( see figure 2)
Nerve Supply
The common fibular nerve supplies the joint.( see figure 2)
Movements
A small amount of gliding movement takes place during movements at the ankle joint.
Relations
The common fibular nerve runs posterior to the head of the fibula, medial to the tendon of biceps femoris, which is closely associated with the anterior capsule. The anterior and posterior tibial branches of the popliteal artery, and the fibular artery are all vulnerable inferomedial to the joint. ( see figure 2)
Injury of proximal tibiofibular joint
Dislocation of the Proximal Tibiofibular Joint
A proximal tibiofibular joint dislocation is a rare and often missed diagnosis. It accounts for <1% of all knee injuries.
The typical mechanism of injury is a fall onto an adducted and flexed knee . They can also occur as a result of high-energy trauma.
Common clinical features include inability to weight-bear, lateral knee pain and tenderness/prominence of the fibular head.
This type of injury is typically treated with a closed reduction (a reduction is a procedure to restore the joint to its natural alignment). Complications of proximal tibiofibular joint dislocation include common fibular nerve injury (the nerve winds around the neck of the fibula), and recurrent dislocation.
The typical mechanism of injury is a fall onto an adducted and flexed knee . They can also occur as a result of high-energy trauma.
Common clinical features include inability to weight-bear, lateral knee pain and tenderness/prominence of the fibular head.
This type of injury is typically treated with a closed reduction (a reduction is a procedure to restore the joint to its natural alignment). Complications of proximal tibiofibular joint dislocation include common fibular nerve injury (the nerve winds around the neck of the fibula), and recurrent dislocation.

Dislocation of the Proximal Tibiofibular Joint
Acute proximal tibiofibular joint dislocation: a sports related injury
Case presentation
A 19-year-old male soccer player presented to emergency room after twisting his left knee. When suddenly changing the direction with his left foot fixed to the ground, he felt an acute knee pain being unable to weight bear.
The patient presented with a protruding fibular head (Figure 3) with pain on direct palpation, and was unable to fully extend the injured knee, holding it in a 10-degree flexion position. No signs of joint effusion, meniscus injuries, instability or neurovascular disorders. There was no pain in ipsilateral ankle or hip joint, with full range of motion. Contralateral knee showed no alterations when performing physical examination.
A 19-year-old male soccer player presented to emergency room after twisting his left knee. When suddenly changing the direction with his left foot fixed to the ground, he felt an acute knee pain being unable to weight bear.
The patient presented with a protruding fibular head (Figure 3) with pain on direct palpation, and was unable to fully extend the injured knee, holding it in a 10-degree flexion position. No signs of joint effusion, meniscus injuries, instability or neurovascular disorders. There was no pain in ipsilateral ankle or hip joint, with full range of motion. Contralateral knee showed no alterations when performing physical examination.
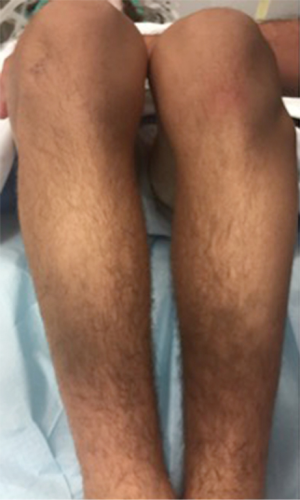
Protruding fibular head.
Plain radiographs (AP and lateral) were obtained revealing an isolated antero-lateral PTFJ dislocation (Ogden type II) (Figure 4). CT scan corroborated this diagnosis (Figure 5).
.png)
Radiographs show a type II dislocation
.png)
CT scan corroborate initial findings.
Closed reduction under general anesthesia was performed successfully. With patient under general anesthesia in supine position, the knee was held in a flexion (relaxing femoral biceps tendon, lateral collateral ligaments) and ankle eversion and dorsiflexion were performed (relaxing the anterolateral compartment muscles and interosseous membrane), followed by a direct AP manual pressure over fibular head, until a “pop” was heard. Immediate post-reduction radiographs were obtained to confirm the anatomical reduction (Figure 6) as well as a MRI, excluding concomitant injuries. A Robert-Jones type immobilization was applied and weight bearing was limited for the first 3 weeks with a gradual return to full weight bearing over 6 weeks—no complaints at that time. General rehabilitation program was followed. Return to play with no restrictions was possible after 3 months.
.png)
Radiographs after close reduction.
*How to perform a reduction of a proximal trio fibular joint dislocation? ( see video below)
2-Distal Tibiofibular Joint
Definition
Distal Tibiofibular Joint
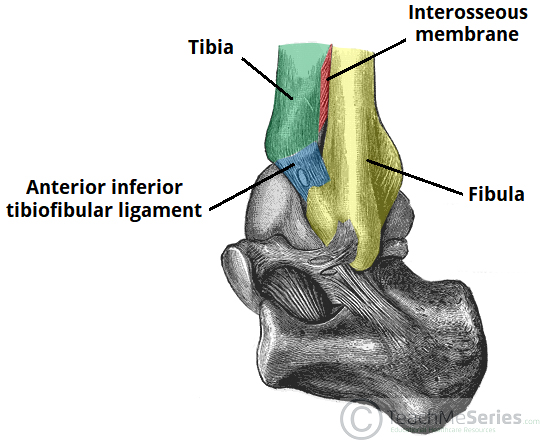
Articulation is between the fibular notch at the lower end of the tibia and the lower end of the fibula The opposed bony surfaces are roughened.(see figure 7)
Type
The distal tibiofibular joint is a fibrous joint.
Capsule
There is no capsule.
Ligaments
The interosseous ligament is a strong, thick band of fibrous tissue that binds the two bones together. The interosseous membrane , which connects the shafts of the tibia and fibula together, also greatly strengthens the joint .
The anterior and posterior ligaments are flat bands of fibrous tissue connecting the two bones together in front and behind the interosseous ligament.
The inferior transverse ligament runs from the medial surface of the upper part of the lateral malleolus to the posterior border of the lower end of the tibia .( see figure 7)
Nerve Supply
Deep fibular and tibial nerves supply the joint.
Movements
A small amount of movement takes place during movements at the ankle joint.
Articulation is between the fibular notch at the lower end of the tibia and the lower end of the fibula The opposed bony surfaces are roughened.(see figure 7)
Type
The distal tibiofibular joint is a fibrous joint.
Capsule
There is no capsule.
Ligaments
The interosseous ligament is a strong, thick band of fibrous tissue that binds the two bones together. The interosseous membrane , which connects the shafts of the tibia and fibula together, also greatly strengthens the joint .
The anterior and posterior ligaments are flat bands of fibrous tissue connecting the two bones together in front and behind the interosseous ligament.
The inferior transverse ligament runs from the medial surface of the upper part of the lateral malleolus to the posterior border of the lower end of the tibia .( see figure 7)
Nerve Supply
Deep fibular and tibial nerves supply the joint.
Movements
A small amount of movement takes place during movements at the ankle joint.
injury of distal tibiofibular joint:
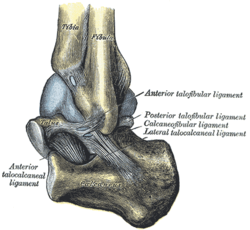
Distal tibiofibular joint and its related ligament are involved with a lot of ankle joint injuries , the most common one is :
ANKLE SYNDESMOSIS - DISTAL TIBIOFIBULAR JOINT OR HIGH ANKLE STRAIN :
What is a high ankle sprain?
A high ankle sprain is when you tear or damage the high ankle ligaments that connect the tibia to the fibula. These ligaments are known as syndesmosis, even though that word refers to the joint itself. You might hear your high ankle sprain called a syndesmotic injury.
Our ankles connect the leg bones to the foot bones. There is an upper ankle and a lower ankle. The upper ankle is the tibia and fibula. In between the upper ankle and lower ankle is the talus, which fits into the arch of the other two bones.
(see figure 8)
Ligaments are tissues made up of fibers (threads) that connect bones to other bones.
A high ankle sprain is when you tear or damage the high ankle ligaments that connect the tibia to the fibula. These ligaments are known as syndesmosis, even though that word refers to the joint itself. You might hear your high ankle sprain called a syndesmotic injury.
Our ankles connect the leg bones to the foot bones. There is an upper ankle and a lower ankle. The upper ankle is the tibia and fibula. In between the upper ankle and lower ankle is the talus, which fits into the arch of the other two bones.
(see figure 8)
Ligaments are tissues made up of fibers (threads) that connect bones to other bones.

What is the difference between a high ankle sprain and a low ankle sprain?
The differences between a high ankle sprain and a low ankle sprain aren’t just location. High ankle sprains involve turning inward or outward while your foot is flexed up. Most low ankle sprains happen when the ankle rolls inward, while other low ankle sprains happen when the ankle rolls outward. The low ankle sprains don’t involve the high ankle ligaments. Low ankle sprains are what most of us think of when we hear someone has a sprained ankle.
What ligaments are involved in a high ankle sprain?
The ligaments that can be damaged or torn in a high ankle sprain include:
• The anterior inferior tibiofibular ligament: This is found in front of the tibia and fibula.
• The posterior inferior tibiofibular ligament: This is found in back of the tibia and fibula.
• The interosseous membrane: This membrane stabilizes the tibia and fibula because it’s located in the middle space between the two bones.
Any of these ligaments can be stretched, torn partially or torn completely in a high ankle sprain.
How common is a high ankle sprain?
A high ankle sprain is less common than a low ankle sprain. High ankle sprains often happen in athletes who play:
• Football.
• Basketball.
• Wrestling.
• Ice hockey.
• Skiing.
• Soccer.
SYMPTOMS AND CAUSES
What are the symptoms of a high ankle sprain?
Symptoms of high ankle sprain include:
• Some swelling.
• Inability to bear weight on the injury, making actions like climbing stairs difficult.
• Inability to walk on your toes.
• Bruising that starts days after the injury.
What causes high ankle sprains?
A high ankle sprain happens when your ankle is hurt when your foot is flexed upward and then twisted either inwards or outwards. It almost always happens as a result of some type of collision, not simply the rolling motion that causes other ankle sprains. High ankle sprains almost always happen when you’re running or jumping.
DIAGNOSIS AND TESTS
How is a high ankle sprain diagnosed?
The first thing your provider will do is to ask questions about why you’re there and get your medical history. Then they’ll do a physical examination.
To diagnose a high ankle sprain, your provider is likely to:
• Have you sit down with your knee bent and leg and foot hanging down. They’ll push up on your foot and twist it a little toward the outside. If there’s a lot of pain, it’s likely that you have a high ankle sprain. Your provider might want to do this test a few days after you’ve had your injury.
• Do the syndesmosis squeeze test. They’ll squeeze your tibia and fibula together, putting pressure on the membrane that separates the two bones (the interosseous membrane). If you feel pain higher up on your leg, you probably have a high ankle sprain.
• Press on the interosseous membrane to find out if you have pain.
• Press on the ligament across the front of your ankle to see if there is pain.
• Order imaging tests, such as X-rays, magnetic resonance imaging (MRI) scans, computed tomography (CT) scans and even possibly ultrasounds. The MRI is the best test for a high ankle sprain, but your provider might use X-rays to rule out other injuries.
MANAGEMENT AND TREATMENT
How is a high ankle sprain treated?
• You can begin treating your ankle injury by following the R.I.C.E. advice: rest, ice, compression (bandaging) and elevation (keeping your foot up) for about three to five days. You might need to use crutches when you need to move.
• You can use over-the-counter non-steroidal anti-inflammatory drugs (NSAIDS) to help with pain and swelling. NSAIDs are available in oral forms like pills and tablets, or topical forms like lotions, creams or sprays.
• Your provider might recommend a brace, tape, or even some type of cast to help you avoid bending your ankle up toward your body.
• Your provider might also recommend physical therapy, including the use of therapeutic bands or exercising in water. Being in water will lessen the amount of weight your ankle has to bear.
• You’re unlikely to need surgery to treat a high ankle sprain unless the damage is very severe or if your ankle continues to be unstable.
watch this videos : first one about how to tape
and the second one about general treatment
The differences between a high ankle sprain and a low ankle sprain aren’t just location. High ankle sprains involve turning inward or outward while your foot is flexed up. Most low ankle sprains happen when the ankle rolls inward, while other low ankle sprains happen when the ankle rolls outward. The low ankle sprains don’t involve the high ankle ligaments. Low ankle sprains are what most of us think of when we hear someone has a sprained ankle.
What ligaments are involved in a high ankle sprain?
The ligaments that can be damaged or torn in a high ankle sprain include:
• The anterior inferior tibiofibular ligament: This is found in front of the tibia and fibula.
• The posterior inferior tibiofibular ligament: This is found in back of the tibia and fibula.
• The interosseous membrane: This membrane stabilizes the tibia and fibula because it’s located in the middle space between the two bones.
Any of these ligaments can be stretched, torn partially or torn completely in a high ankle sprain.
How common is a high ankle sprain?
A high ankle sprain is less common than a low ankle sprain. High ankle sprains often happen in athletes who play:
• Football.
• Basketball.
• Wrestling.
• Ice hockey.
• Skiing.
• Soccer.
SYMPTOMS AND CAUSES
What are the symptoms of a high ankle sprain?
Symptoms of high ankle sprain include:
• Some swelling.
• Inability to bear weight on the injury, making actions like climbing stairs difficult.
• Inability to walk on your toes.
• Bruising that starts days after the injury.
What causes high ankle sprains?
A high ankle sprain happens when your ankle is hurt when your foot is flexed upward and then twisted either inwards or outwards. It almost always happens as a result of some type of collision, not simply the rolling motion that causes other ankle sprains. High ankle sprains almost always happen when you’re running or jumping.
DIAGNOSIS AND TESTS
How is a high ankle sprain diagnosed?
The first thing your provider will do is to ask questions about why you’re there and get your medical history. Then they’ll do a physical examination.
To diagnose a high ankle sprain, your provider is likely to:
• Have you sit down with your knee bent and leg and foot hanging down. They’ll push up on your foot and twist it a little toward the outside. If there’s a lot of pain, it’s likely that you have a high ankle sprain. Your provider might want to do this test a few days after you’ve had your injury.
• Do the syndesmosis squeeze test. They’ll squeeze your tibia and fibula together, putting pressure on the membrane that separates the two bones (the interosseous membrane). If you feel pain higher up on your leg, you probably have a high ankle sprain.
• Press on the interosseous membrane to find out if you have pain.
• Press on the ligament across the front of your ankle to see if there is pain.
• Order imaging tests, such as X-rays, magnetic resonance imaging (MRI) scans, computed tomography (CT) scans and even possibly ultrasounds. The MRI is the best test for a high ankle sprain, but your provider might use X-rays to rule out other injuries.
MANAGEMENT AND TREATMENT
How is a high ankle sprain treated?
• You can begin treating your ankle injury by following the R.I.C.E. advice: rest, ice, compression (bandaging) and elevation (keeping your foot up) for about three to five days. You might need to use crutches when you need to move.
• You can use over-the-counter non-steroidal anti-inflammatory drugs (NSAIDS) to help with pain and swelling. NSAIDs are available in oral forms like pills and tablets, or topical forms like lotions, creams or sprays.
• Your provider might recommend a brace, tape, or even some type of cast to help you avoid bending your ankle up toward your body.
• Your provider might also recommend physical therapy, including the use of therapeutic bands or exercising in water. Being in water will lessen the amount of weight your ankle has to bear.
• You’re unlikely to need surgery to treat a high ankle sprain unless the damage is very severe or if your ankle continues to be unstable.
watch this videos : first one about how to tape
and the second one about general treatment
How long does a high ankle sprain take to heal?
#/ /#
It might take you six to eight weeks to recover from a high ankle sprain. If you’re an athlete, your return to play might take an even longer time. Low ankle sprains generally heal quicker than this.
PREVENTION
How can I reduce my risk of a high ankle sprain?
Ankle sprains are accidents, and there’s no way to prevent accidents completely.
However, there are some things you can do that may make a high ankle sprain less likely to happen. You can:
• Follow an exercise program that will make your joints stronger and more flexible.
• Follow an exercise program that will improve your balance and your ability to sense how your body is positioned (proprioception). Proprioception is part of your balance and is the way that your brain knows how your body is positioned.
• Use protective equipment like braces or tape to protect your ankles.
OUTLOOK / PROGNOSIS
What is the outlook (prognosis) for a high ankle sprain?
The outlook is good for recovering from a high ankle sprain, most often using only non-surgical methods. However, you’ll probably be more prone to injuring your ankle again. Also, you may have stiffness in the joint later on.
LIVING WITH
When should I see my healthcare provider for a high ankle sprain?
If you’ve hurt your foot and you can’t put any weight on it, you should call your provider or go to an emergency room. You’ll want to find out if you have any broken bones. You’ll need to follow your provider’s instructions on the best way to take care of the injury.
*A NOTE FROM CLINIC
Most of us have probably twisted a foot and ended up with a sprained ankle. If you have been participating in an activity that involves jumping or running and you hurt your ankle, you might find you have a high ankle sprain. Make sure that you follow your healthcare provider’s instructions so that you heal completely
*WATCH THIS VIDEO
#/ /#
It might take you six to eight weeks to recover from a high ankle sprain. If you’re an athlete, your return to play might take an even longer time. Low ankle sprains generally heal quicker than this.
PREVENTION
How can I reduce my risk of a high ankle sprain?
Ankle sprains are accidents, and there’s no way to prevent accidents completely.
However, there are some things you can do that may make a high ankle sprain less likely to happen. You can:
• Follow an exercise program that will make your joints stronger and more flexible.
• Follow an exercise program that will improve your balance and your ability to sense how your body is positioned (proprioception). Proprioception is part of your balance and is the way that your brain knows how your body is positioned.
• Use protective equipment like braces or tape to protect your ankles.
OUTLOOK / PROGNOSIS
What is the outlook (prognosis) for a high ankle sprain?
The outlook is good for recovering from a high ankle sprain, most often using only non-surgical methods. However, you’ll probably be more prone to injuring your ankle again. Also, you may have stiffness in the joint later on.
LIVING WITH
When should I see my healthcare provider for a high ankle sprain?
If you’ve hurt your foot and you can’t put any weight on it, you should call your provider or go to an emergency room. You’ll want to find out if you have any broken bones. You’ll need to follow your provider’s instructions on the best way to take care of the injury.
*A NOTE FROM CLINIC
Most of us have probably twisted a foot and ended up with a sprained ankle. If you have been participating in an activity that involves jumping or running and you hurt your ankle, you might find you have a high ankle sprain. Make sure that you follow your healthcare provider’s instructions so that you heal completely
*WATCH THIS VIDEO
3- Middle tibiofibular joint (interosseous membrane of the leg)
Definition
The Interosseous Membrane Of The Leg
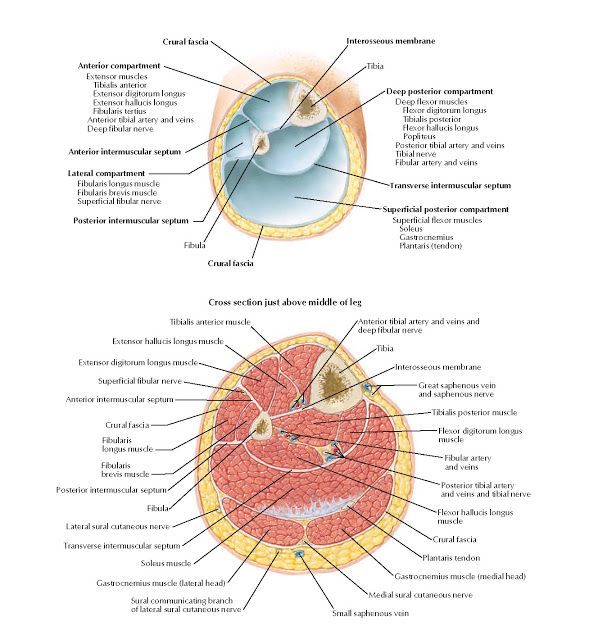
The Lower or distal interosseous membrane spans between the tibia and fibula and divides the lower leg into compartments and provides an anchor point for several muscles of the distal leg to attach. The deep peroneal nerve travels through the interosseous membrane to supply the extensors of the leg.
This membrane can be injured when the joints experience high stress during a sudden twisting motion. This often occurs when an athlete is wearing cleats, and the ankle is forced violently outwards. This is known as a syndesmotic ankle sprain or a high ankle sprain.(see figure 9)
The Lower or distal interosseous membrane spans between the tibia and fibula and divides the lower leg into compartments and provides an anchor point for several muscles of the distal leg to attach. The deep peroneal nerve travels through the interosseous membrane to supply the extensors of the leg.
This membrane can be injured when the joints experience high stress during a sudden twisting motion. This often occurs when an athlete is wearing cleats, and the ankle is forced violently outwards. This is known as a syndesmotic ankle sprain or a high ankle sprain.(see figure 9)
Related structures
It is in relation, in front , with the Tibialis anterior, Extensor digitorum longus, Extensor hallucis proprius, Peronæus tertius, and the anterior tibial vessels and deep peroneal nerve; behind , with the Tibialis posterior and Flexor hallucis longus. (see figure 10)
Injury of Middle tibiofibular joint (interosseous membrane of the leg)
An injury to the interosseous membrane can alter the function and anatomic stability of either the forearm or the leg. Membrane injury can cause fibrous (scar tissue), instability of both the joints and the muscles that attach to them.
Injuries can cause ossification or the need for a surgical release of scar tissue known as *tenolysis . Entrapment of the nerve or artery can occur as well causing strength loss, numbness, or tingling.
*Tenolysis is a surgical procedure to release or free a tendon from adhesions. Sometimes as a result of an injury or surgery, the tendons that bend and straighten the fingers become stuck in the scar tissue (adhesions) preventing the finger from moving properly.
Injuries can cause ossification or the need for a surgical release of scar tissue known as *tenolysis . Entrapment of the nerve or artery can occur as well causing strength loss, numbness, or tingling.
*Tenolysis is a surgical procedure to release or free a tendon from adhesions. Sometimes as a result of an injury or surgery, the tendons that bend and straighten the fingers become stuck in the scar tissue (adhesions) preventing the finger from moving properly.
Ossification of the Interosseous Membrane of the Leg in a Football Player: Case Report
. We report a case of ossification of the interosseous membrane (OIM) of the leg in a football player who had no history of severe local traumas. A review of the literature of the OIM of the leg in athletes was also carried out. Case Report . A 38-year-old Caucasian male patient complained of pain on lateral aspect of the leg when playing football. Pain progressively worsened until he had to stop the sporting activity. Radiographs, and then CT and MRI, showed OIM in the middle third of the left leg. MRI showed inflammation of tibia periosteum and bone adjacent to the ossification, which was then excised. Two months after surgery the patient returned to play football. Conclusion . A thorough analysis of the literature revealed three types of OIM of the leg in athletes. Type I usually occurs after a syndesmosis ankle sprain, Type II appears to result from a tibia fracture, and Type III, of which only one fully recorded case has been published, is probably caused, as in our patient, by repetitive minor traumas to the leg. Awareness of the existence of Type III OIM can avoid erroneous diagnoses leading to useless investigations and treatments.
Introduction
Heterotopic ossification consists in bone formation outside the skeleton. The most typical form of heterotopic ossification, unrelated to surgical procedures, neurologic injuries, or tumors, is myositis ossificans circumscripta, which usually occurs after a trauma but can even be initiated by multiple minor injuries or develop spontaneously [1]. Ossification of the interosseous membrane (OIM) of the leg may exhibit some features similar to those of myositis ossificans.(see figure 11)
Introduction
Heterotopic ossification consists in bone formation outside the skeleton. The most typical form of heterotopic ossification, unrelated to surgical procedures, neurologic injuries, or tumors, is myositis ossificans circumscripta, which usually occurs after a trauma but can even be initiated by multiple minor injuries or develop spontaneously [1]. Ossification of the interosseous membrane (OIM) of the leg may exhibit some features similar to those of myositis ossificans.(see figure 11)

Reference:
• Snell’s clinical anatomy by regions, LAWRENCE E. WINESKI, PhD, TENTH EDITION, 1408-1411.
• High Ankle Sprain, Cleveland clinic,
• https://my.clevelandclinic.org/health/diseases/22249-high-ankle-sprains
• The Interosseous Membrane Of The Leg, Dr. Justin Dean , https://drjustindean.com/interosseous/
• Ossification of the Interosseous Membrane of the Leg in a Football Player, Hitesh N. Modi, hindawi, https://www.hindawi.com/journals/crior/2016/2930324/
• High Ankle Sprain (Syndesmotic Sprain), By Terry Zeigler, EdD, ATC , sportsmd, https://www.sportsmd.com/sports-injuries/foot-ankle-injuries/high-ankle-sprain-syndesmotic-sprain/
• poroximal tibiofibular joint, Schnell D'Sa, teachmeanatomy, https://teachmeanatomy.info/lower-limb/joints/tibiofibular-joints/
• High Ankle Sprain, Cleveland clinic,
• https://my.clevelandclinic.org/health/diseases/22249-high-ankle-sprains
• The Interosseous Membrane Of The Leg, Dr. Justin Dean , https://drjustindean.com/interosseous/
• Ossification of the Interosseous Membrane of the Leg in a Football Player, Hitesh N. Modi, hindawi, https://www.hindawi.com/journals/crior/2016/2930324/
• High Ankle Sprain (Syndesmotic Sprain), By Terry Zeigler, EdD, ATC , sportsmd, https://www.sportsmd.com/sports-injuries/foot-ankle-injuries/high-ankle-sprain-syndesmotic-sprain/
• poroximal tibiofibular joint, Schnell D'Sa, teachmeanatomy, https://teachmeanatomy.info/lower-limb/joints/tibiofibular-joints/